Back Pain | Ankylosing Spondylitis | Cases
Published on Jan 20, 2021
26 ♂
- Presented to MSK service with back pain.
- Gave a 7 year history of back pain (started aged 19)
- Seen previously in MSK service 5 years ago (aged 21). Had an MRI scan which was normal.
- Has has physiotherapy in the past.
- Has been regularly having chiropractic treatment.
- Reports that his back remains arched when he is lying supine (lordosis doesn’t obliterate when lying).
- Pain disturbs sleep.
- Stiff for approximately 30 mins in the morning.
- No P+N or Numbness or any Bladder / Bowel issues.
- Desk-based (occupation)
- Goes to a gym. Has been doing core work. Can’t do dead lifts. Can manage to do bench press and leg work out. Hasn’t been able to do any sports for past 6 years.
- Taking ibuprofen and paracetamol which help to some extent.
- Reports the pain has been worse over the past 1 year despite having regular chiropractic treatment.
- Chiropractor feels there is something wrong. In his letter he reports patient has exaggerated lumbar lordosis, thoracic kyphosis, inability to flex torso, marked hip restriction with groin pain, tight hams and gastrocnemius. Chiropractor suggests that the patient should be assessed by orthopaedics for scoliosis of progressive nature.
Examination
- Obs: standing – increased lumbar lordosis.
- Lumbar Flexion – nil, bends at hips.
- Extension – nil
- Lateral flexions – nil
- Mild to moderate stiffness in both hips.
- Stiff spine on palpation
- Tender SIJs bilaterally.
Provisional Diagnosis
- Ankylosing Spondylitis (AS).
- No family history
- No lumbar spine movements present – possibly ankylosed
Investigations
- Inflammatory screen including HLA B27.
- MRI SIJ and Lumbar spine.
Results
- CRP: 19
- ESR: 29
- HLA B27: +ve
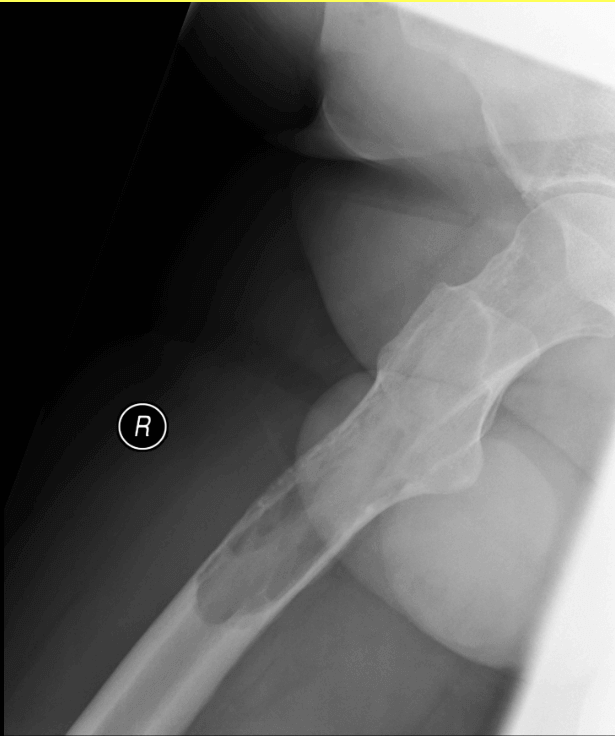
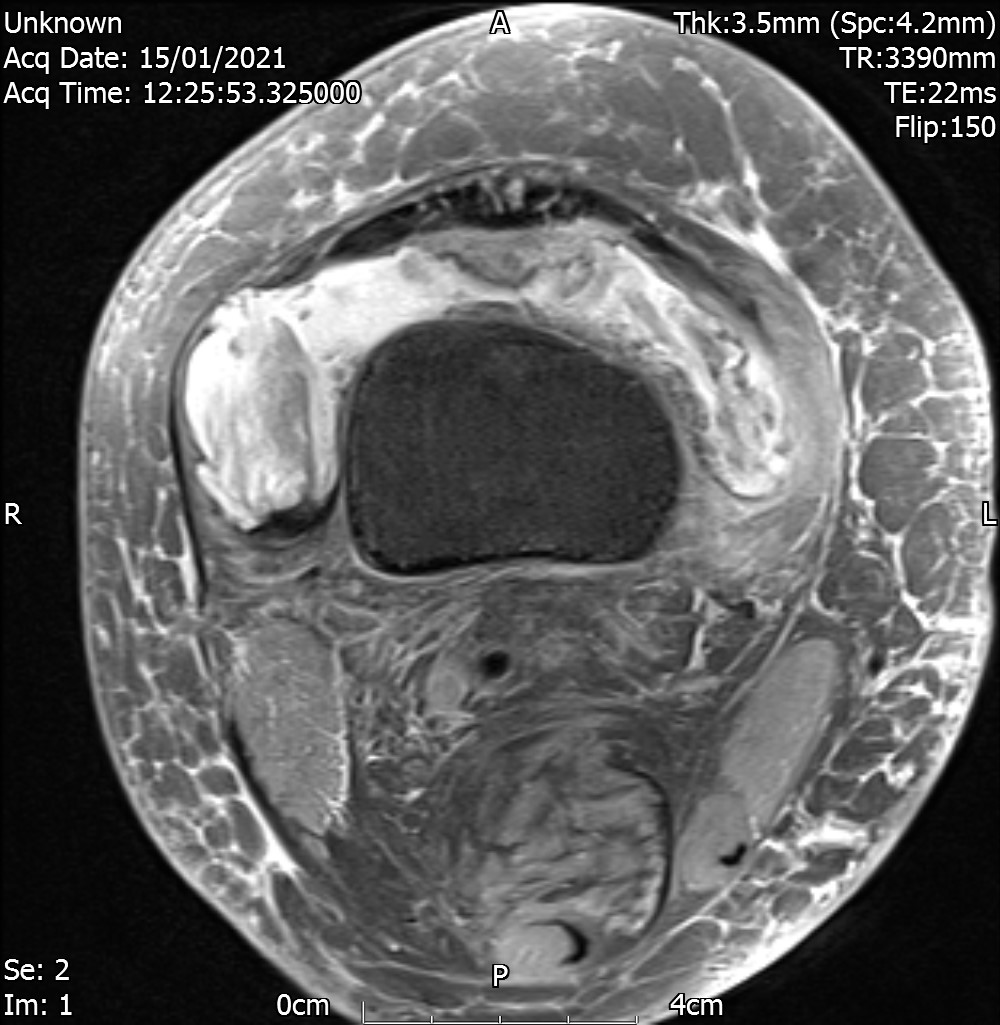
MRI SIJ
There is joint space irregularity demonstrated bilaterally associated with relatively symmetrical areas of subchondral fatty marrow proliferation. Minor subchondral marrow oedema within the superior aspect of the left SI joint and there are also some partial areas of ankylosis demonstrated bilaterally.
CONCLUSION
The overall findings are most in keeping with an established bilateral symmetrical sacroiliitis which is most likely inflammatory in nature. Minor disease activity within the superior aspect of the left SI joint.
Consider a rheumatology opinion and correlation with HLA-B27 status.
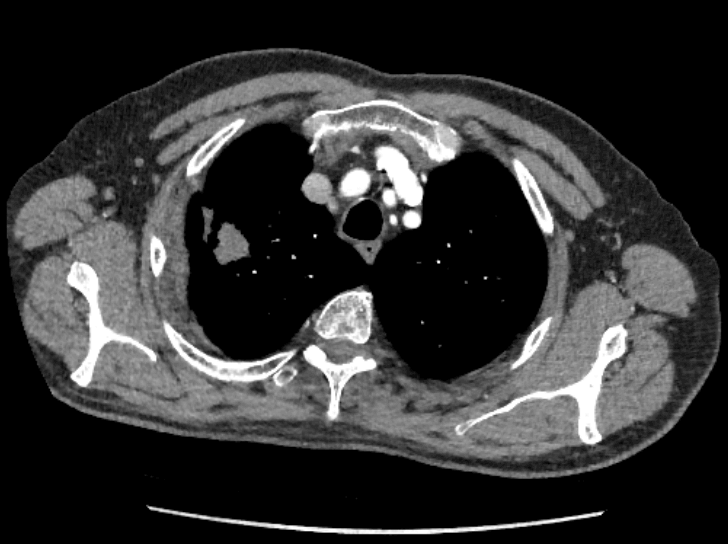
MRI Lumbar Spine
No vertebral body collapse, end-plate destruction or loss of alignment (exaggerated lumbar lordosis).
No infiltrative marrow process. Satisfactory appearances of the visualised pre-and paravertebral soft tissues.
Normal appearances of the visualised cord and conus medullaris.
There are no inflammatory endplate changes. Vertebral bodies are squared.
Axial images acquired from L3-4 through L5-S1 do not demonstrate any significant disc prolapse, neural entrapment or canal stenosis. There is however facet joint disease at L3-4 through L5-S1 with marrow oedema within the right facet joint at L3-4 and the left-sided facet joint at L4-5.
IMPRESSION
Lower lumbar facet joint disease with associated marrow oedema in the facet joints at L3-4 on the right and L4-5 on the left which may be inflammatory in nature given the appearances of the SI joints. No neural compression or canal stenosis.
Analysis
This is a classical case of delay in diagnosis. The delay is more than 7 years in this case.
A study by Moran et al (2016) in Annals of Rheumatic Diseases reported a mean delay of 8-9 years in establishing the diagnosis of AS. They reviewed their AS service data in a district hospital in North West England and results showed the following.
44 males and 9 females with age range 28–83 years.
Mean delay to diagnosis was 8.94 years. Median delay to diagnosis: 8 years.
1962–1999 (10 patients) Mean 6.7 years. Median 7 years
2000–2004 (13 patients) Mean 9.5 years. Median 7 years
2005–2009 (15 patients) Mean 9.8 years. Median 8 years
2010–2015 (16 patients) Mean 9.1 years. Median 7 years
Moran et al 2016 – Delay To Diagnosis in Ankylosing Spondylitis: A Local Perspective
Hamilton et al (2011) in their study reported a diagnostic delay of 8.57 years.
Ref: Services for people with ankylosing spondylitis in the UK–a survey of rheumatologists and patients
Letter to Editor by Sykes et al (Rheumatology 2015) also highlighted this issue of delay in diagnosis.
Information from National Axial Spondyloarthritis Society
26% of people with AS have acute anterior uveitis & 40% of people with acute anterior uveitis have spondyloarthritis.9% of people with AS have psoriasis.
7% of people with AS have inflammatory bowel disease.
NASS website also has educational posters / flyers available for download which can be given to patients.
What is Enthesitis?
What are biologics?
Axial Spondyloarthropathy – AxSpA
- radiaographic – r-AxSpA
- non radiographic – nr-AxSpA
Axial Spondyloarthropathy | associated features, extra-articular manifestations
- Uveitis
- Dactylitis (mainly seen in Psoriatic arthritis)
- Enthesitis (mainly seen in Psoriatic arthritis)
- Psoriasis
- Inflammatory Bowel Disease
Further Reading:
- Axial Spondyloarthritis: Classification vs Diagnostic Criteria – Rheumatology 2020
- Axial spondyloarthritis: new advances in diagnosis and management – BMJ 2020
- Spondyloarthritis Infographic – BMJ
- Spondyloarthritis NICE Guidelines Summary Poster – BMJ
- Axial Spondyloarthritis – One year in review 2018 – Clinical and Experimental Rheumatology