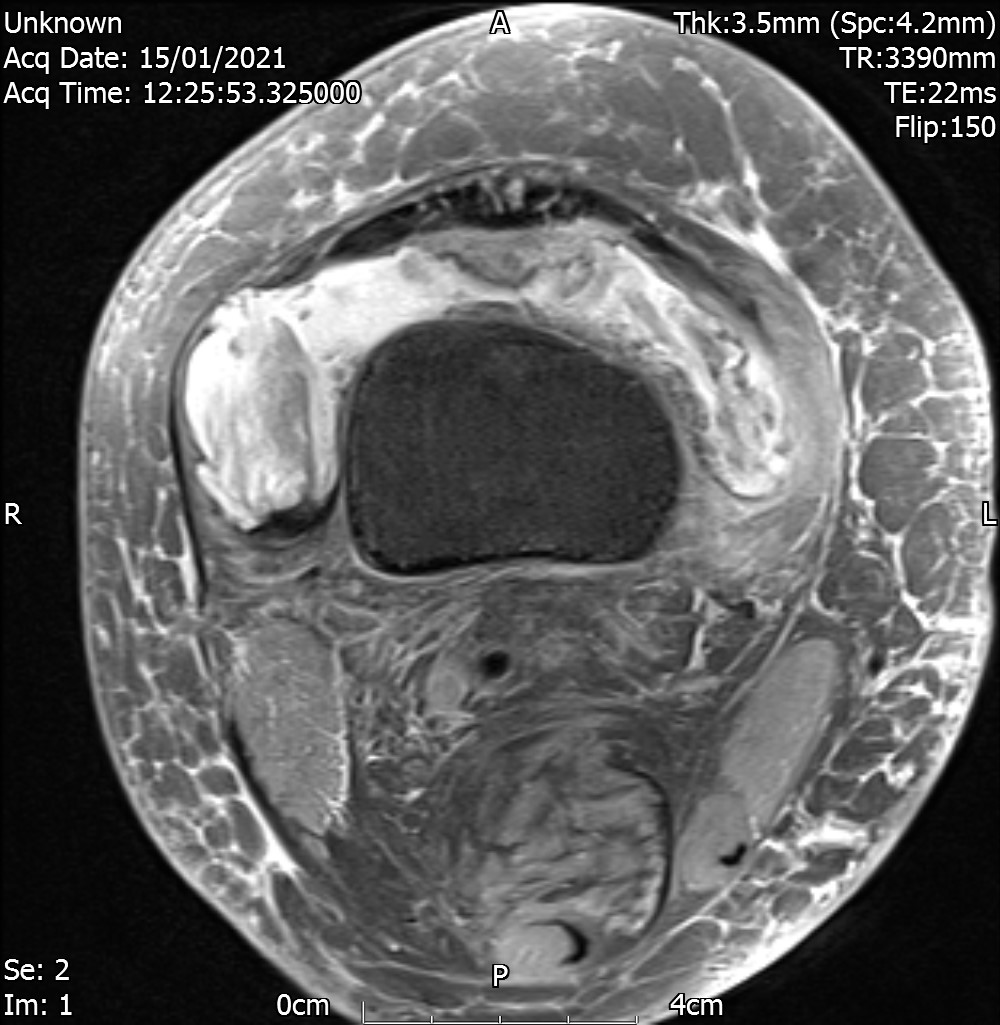
CES – Cauda Equina Syndrome
One red flag is not good enough to act upon.
Todd & Dickson 2016 – CES Groups
- S – Suspected
– B/L radicular pain - I – Incomplete
–Urinary difficulties, altered urinary sensation, loss of desire to void, poor urinary stream, need to strain to micturate. - R – Retention
– Painless urinary retention and overflow incontinence.
– does not improve post surgery. - C – Complete
– Loss of CE function, absent perianal sensation, patulous anus, paralysed bladder and bowel.
– does not improve post surgery.
Diagnosis and treatment of the CESS and the CESI patient will achieve the best outcomes but these are the patients where clinical assessment has poor predictive value. Therefore all patients whose diagnosis is “? CES” (including the CESS patient with bilateral radiculopathy) require urgent MRI.
Nick Todd
Decision Making
- B/L leg pain + CES symptoms -> Emergency referral (check local pathway, refer to A&E). Patient needs MRI asap.
- B/L leg pain but no CES symptoms + Abnormal Neurology i.e. motor deficit 3/5 MRC, significantly deteriorating -> Urgent MRI (within a week). Safety net the patient for CES.
- B/L leg pain + Normal Neurology + No CES symptoms + positive Neurodynamic tests -> Rx as per radicular pain. Safety net these patients. Routine MRI if not improving.
- B/L leg pain + Normal Neurology + No CES symptoms + negative Neurodynamic tests -> Rx as needed and safety net the patient.
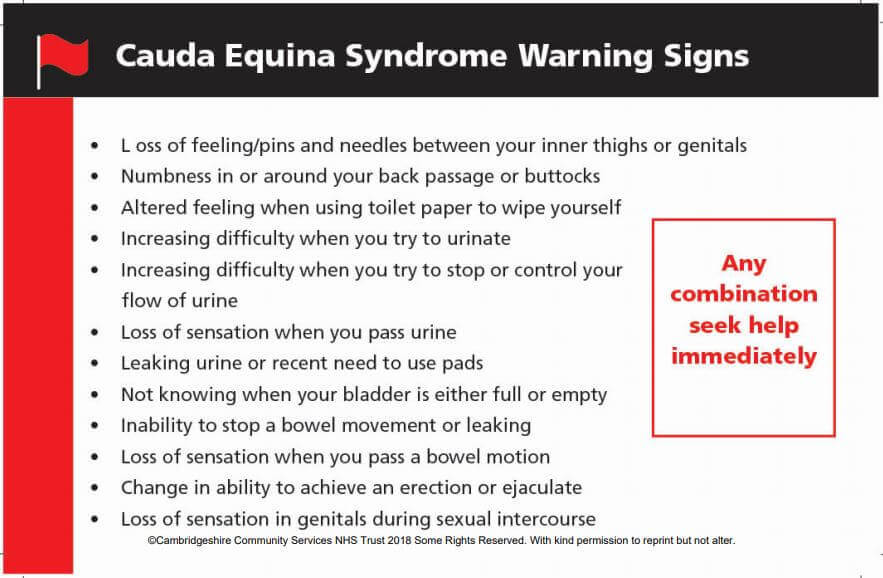
CES – Subjective
History taking is key.
physical tests have very poor reliability and validity in diagnosing CES
– Anal tone not specific for CES. It can be normal in CES and vice versa.
– Bladder scanning. More than 200 ml residual volume post voiding and a +ve MRI scan => CES.
Sexual function questions are key. Explain this to the patient as to why you are asking these questions.
– Q: Men – ability to gain, maintain erection and ejaculate.
– Q: Women – Vaginal sensation present or not + ability to achieve climax.
A helpful CES card enlists majority of the signs / symptoms to screen | Red Flags
General Information Video by CSP
References
- https://e-space.mmu.ac.uk/621393/3/Assessment%20and%20Management%20of%20Cauda%20Equina%20Syndrome.pdf
- International Framework for Spinal Red Flags – JOSPT (2020)
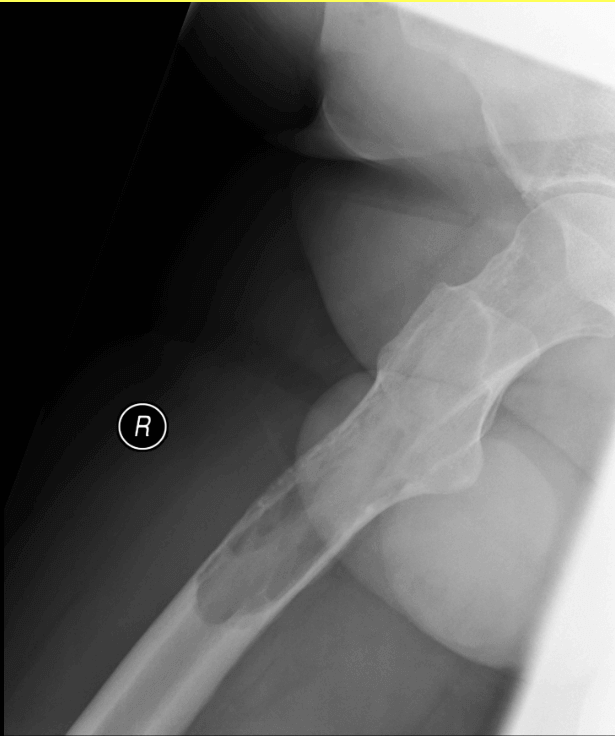
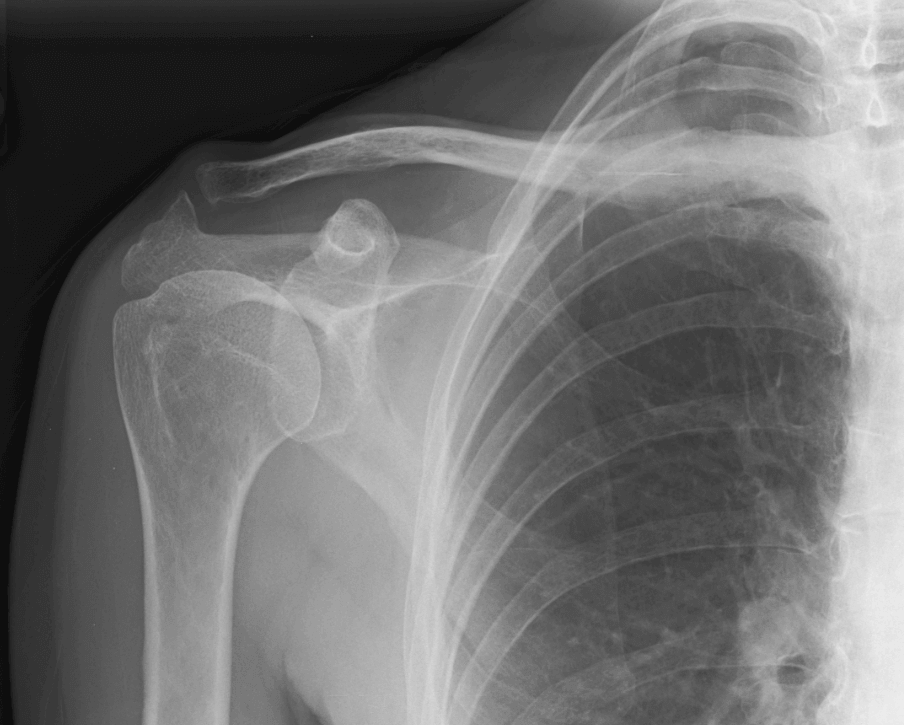
Spinal Fracture
Causes
- Osteoporosis – mainly vertebral stress fracture, common between T8 and L2. 70% of these are undiagnosed, 46% are unreported. 55% women with hip fractures have had a vertebral fracture.
- Metastatic
- Myeloma
- Infection
- Trauma
Risk Factors
- Age > 65
- Sex – females more prone (nearly all women over 70 have sustained a vertebral stress fracture). By the age of 80, 70% females are osteoporotic. 30% females between the ages of 50-70 are osteoporotic.
- Steroid use
- Tumours / Malignancies
- Alcohol consumption
- Smoking – 20 per day
- Hyperparathyroidism
- Bowel issues – absorption problems associated with inflammatory bowel disease, celiac.
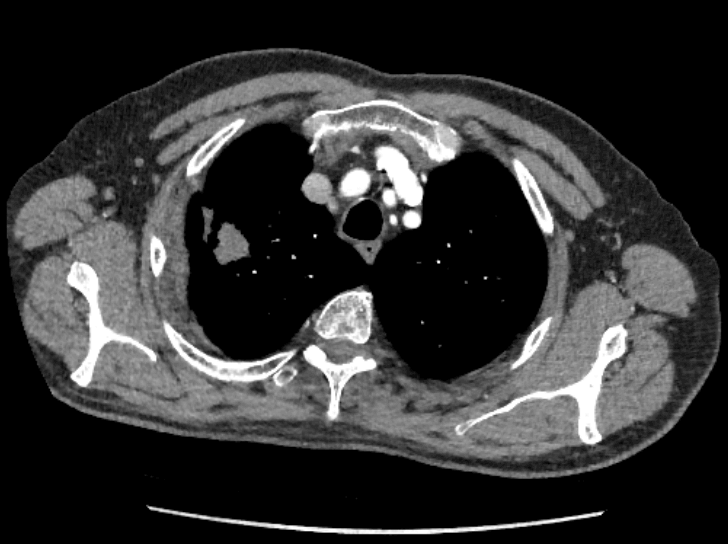
Malignancy / Cancer
BPLTK cancers are the top 5 cancers which metastasise to the Spine.
- BPLTK => Breast, Prostate, Lung, Thyroid, Kidney.
- 30% of these cancers go on to develop mets. 50% of these happen in the first 2 years but can also happen 20 years later.
Distribution
- 70% in Thoracic Spine
- 20% Lumbar Spine
- 10% Cervical Spine
Therefore in cases with previous cancers, whole spine MRI is recommended.
MSCC is the worst case scenario.
However 25% of mets cases do not have a diagnosed primary. So don’t be reassured by absence of history of cancer.
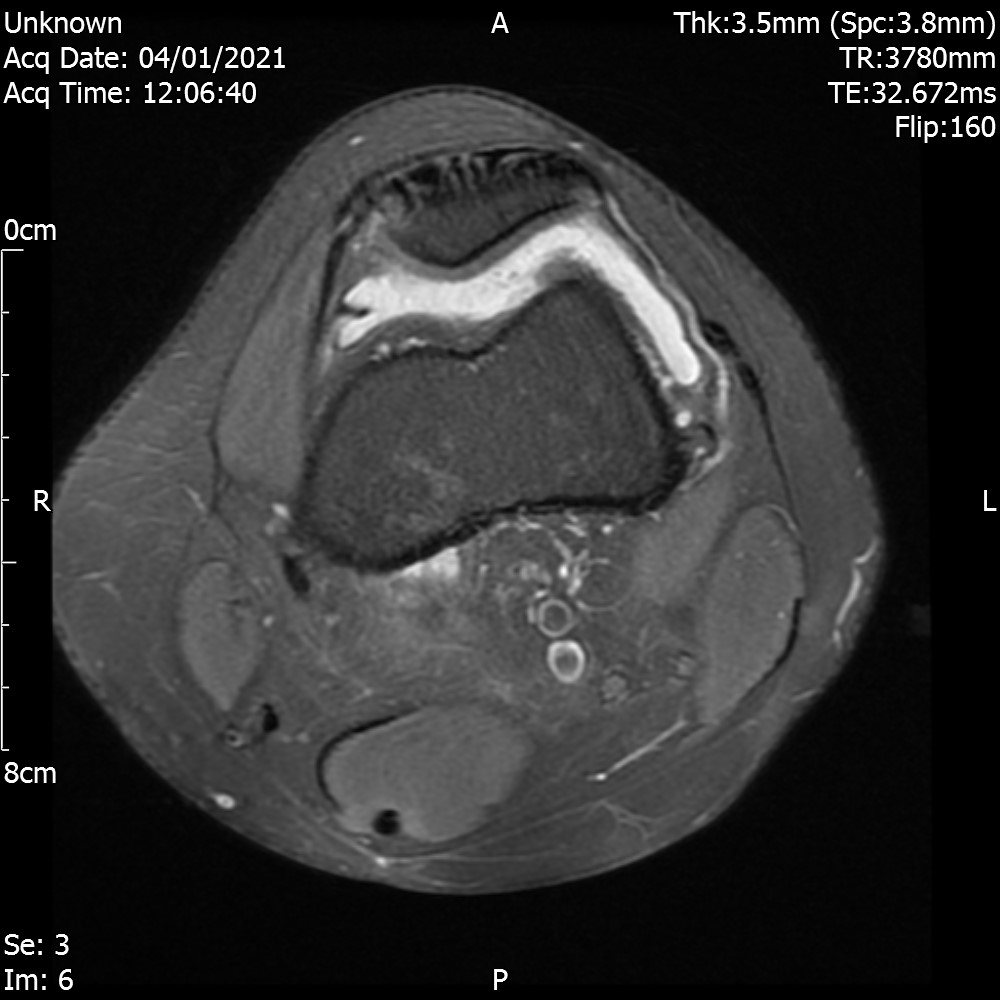
Spinal Infection
Risk Factors | Red Flags
- Sex – Men 70% more likely to have a spinal infection compared to women.
- Immunosuppression – HIV, Cancer, diabetes
- IV drug abuse, obesity, smoking, alcoholism
- preexisting infection, history of TB
Red flags currently used in clinical practice that are considered specific to infection are; the use of corticosteroids, or immunosuppressant therapy, Intravenous drug abuse, past history of TB and fever
Red flags for the early detection of spinal infection in back pain patients
Clinical Features – ‘Classic Triad’
- Spinal pain
- Fever
- Neurological dysfunction
Risk factors i.e. IV drug use, diabetes and cancer have high sensitivity (98%) making them better predictor of spinal infection than clinical features of classic triad.
The review highlights that a number of morbidities such as diabetes, cancer, and HIV are among those conditions associated with immunosuppression which can consequently result in a susceptibility to infection. Determinants such as corticosteroid use and alcohol abuse can also lead to a risk of immunodeficiency . Also of note is that diseases such as rheumatoid arthritis and cancer sufferers treated with medications known to cause immunodeficiency (e.g. Disease-modifying anti-rheumatic drugs (DMARDS), steroids) are also at risk of SI. Determinants for SI (including intravenous drug use, diabetes and cancer) have high sensitivity (98%) and negative predictive value (99%) making them a better predictor of SI than clinical features such as the ‘classic triad’ (spinal pain, fever and neurological dysfunction).
Red flags for the early detection of spinal infection in back pain patients