Lipoma Arborescens | Cases
Published on Dec 17, 2020
(2016) Patient (male) aged 44 attends physical therapy department with right knee pain. He gives a 5 year history of knee pain. He has noticed on and off swelling in the right knee.
The clinician notices high BMI.
On knee exam, there is slight swelling noticed on the knee. ROM is full with slight tightness at end range flexion and extension.
Provisional diagnosis is medial for meniscal irritation. Patient is advised on some exercises and then reviewed a month later. Patient reports some improvement. He is then asked to attend supervised exercise classes.
Patient attends first exercise class and the clinician running the session notices a lump over the medial knee. The suspected lump is non tender and has no signs of inflammation. On questioning, the patient is oblivious to the lump and mentions that he has never noticed it before. The clinician alerts the case holder about the finding.
Meanwhile the patient shifts exercise group sessions to a different one and another clinician addresses the lump. A senior clinician is called in to give an opinion and the senior clinician feels that it is suprapatellar bursitis. The patient continues to attend classes and then misses a session and gets discharged.
2017 – 2020 – Patient continues to get pain and sees his doctor as needed. He manages with pain relief medicines.
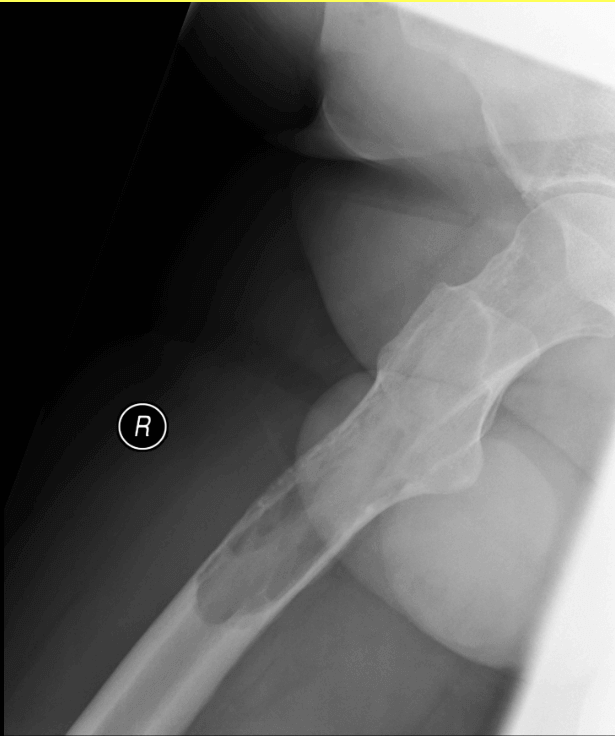
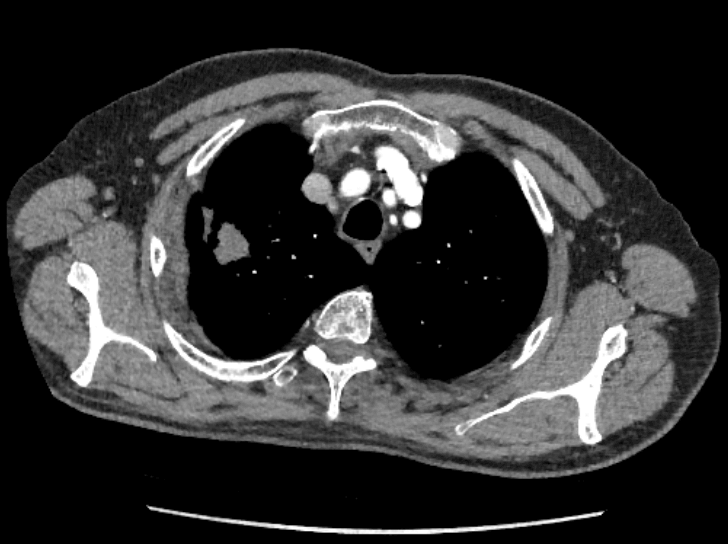
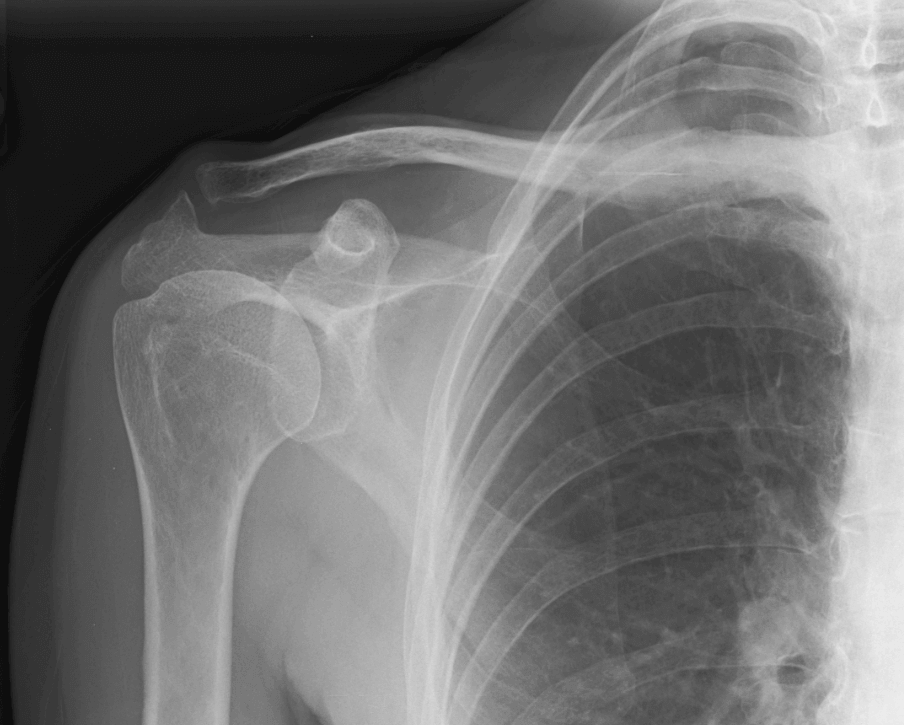
(2020) – Family physician refers the patient to physical therapy for ongoing knee issue. The doctor mentions in the referral that swelling is moderate to severe and the doctor is not sure that he can drain the swelling in his clinic as it might need further follow up. He also arranges an x-ray. Images below.
 |
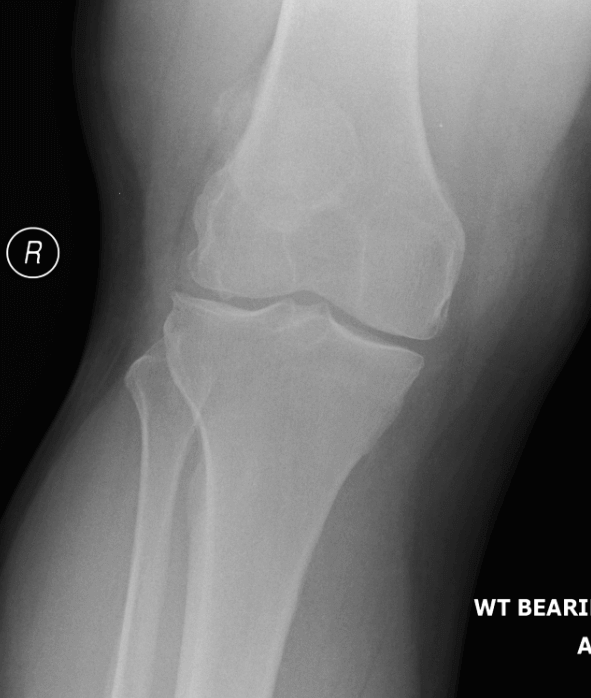 |
Physiotherapist assesses the patient. The clinician mentions swelling in the notes but does not report it as a lump. The knee is reported to have 120° flexion, full extension, intact ligaments and a positive McMurrays. A provisional diagnosis of meniscal degeneration / OA is made. The clinician requests an MRI.
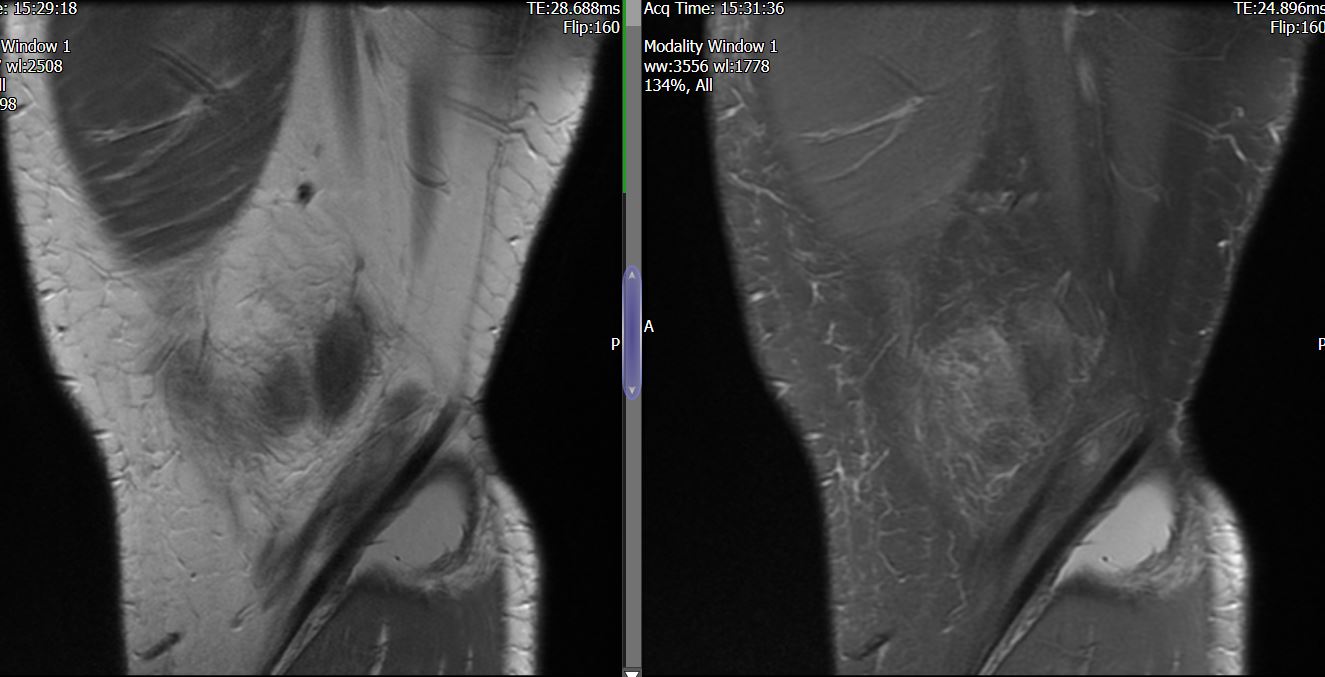
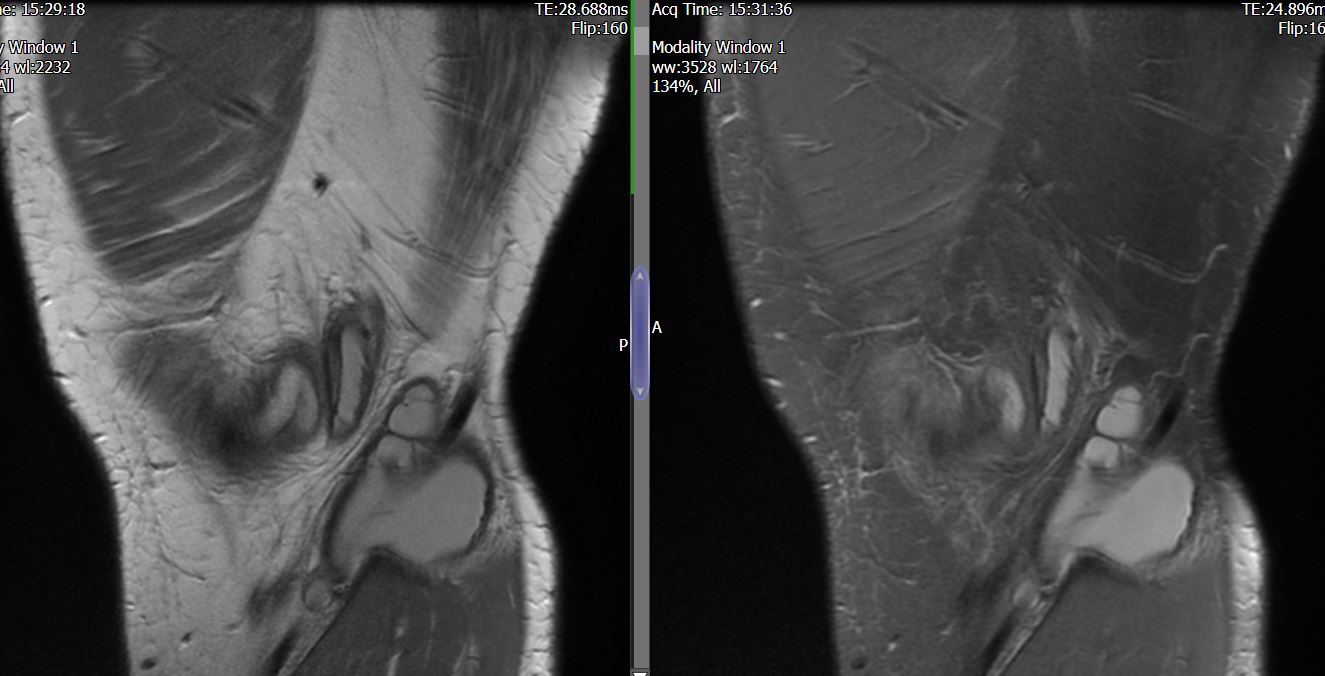
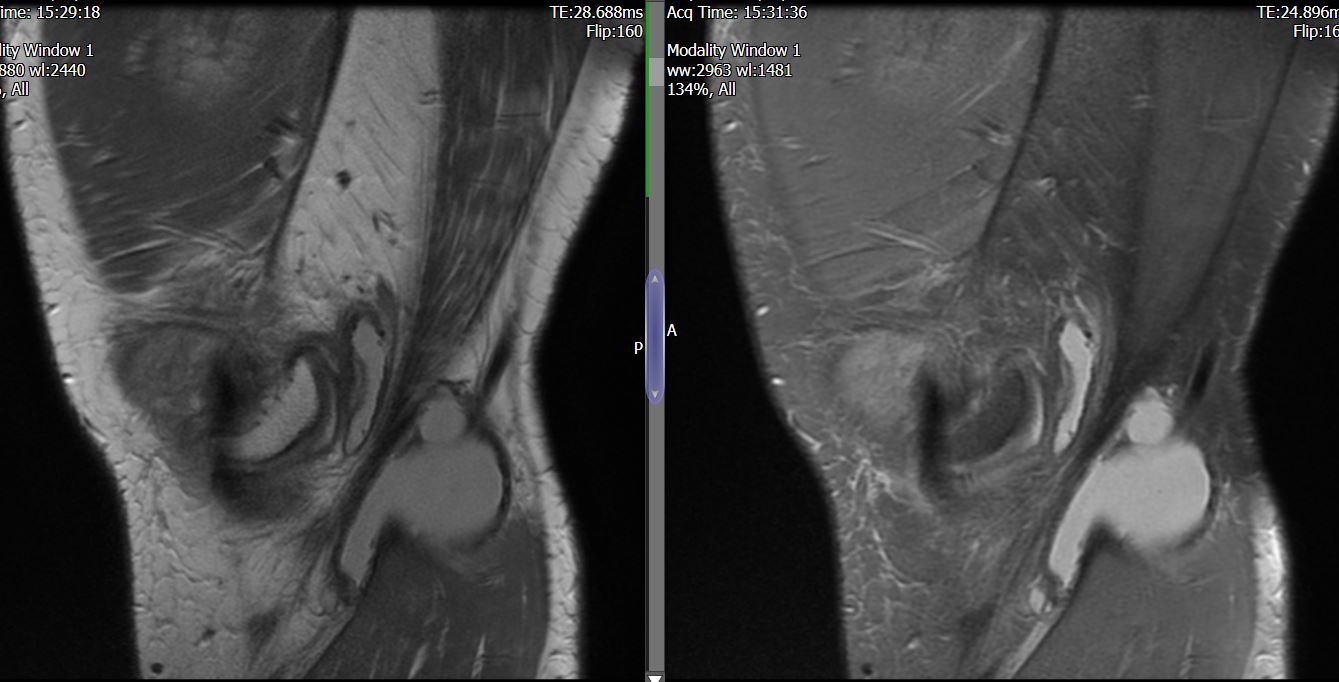
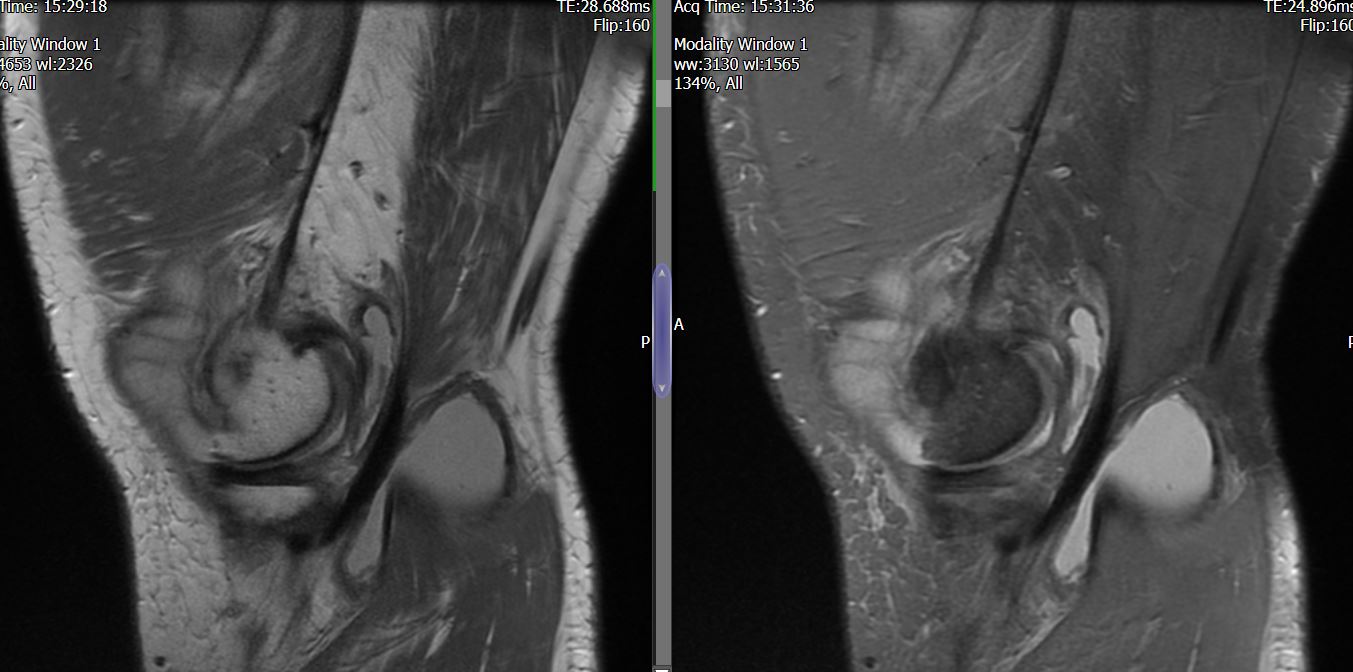
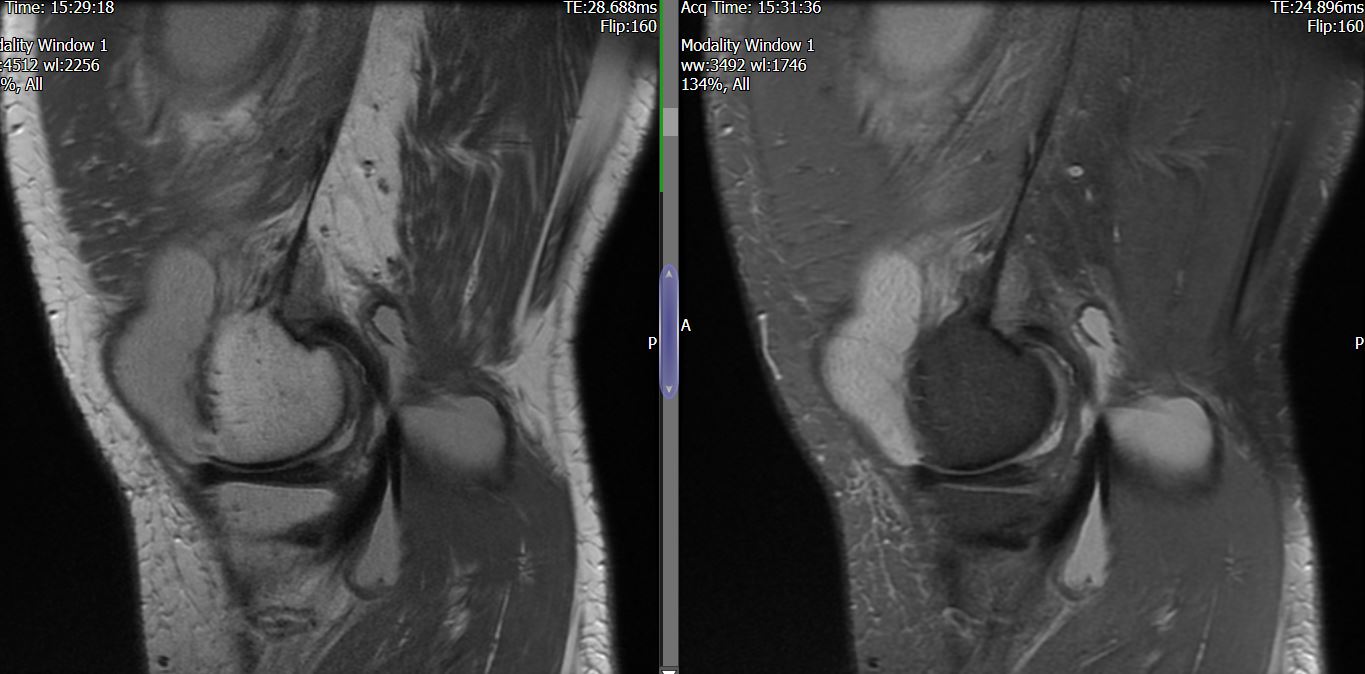
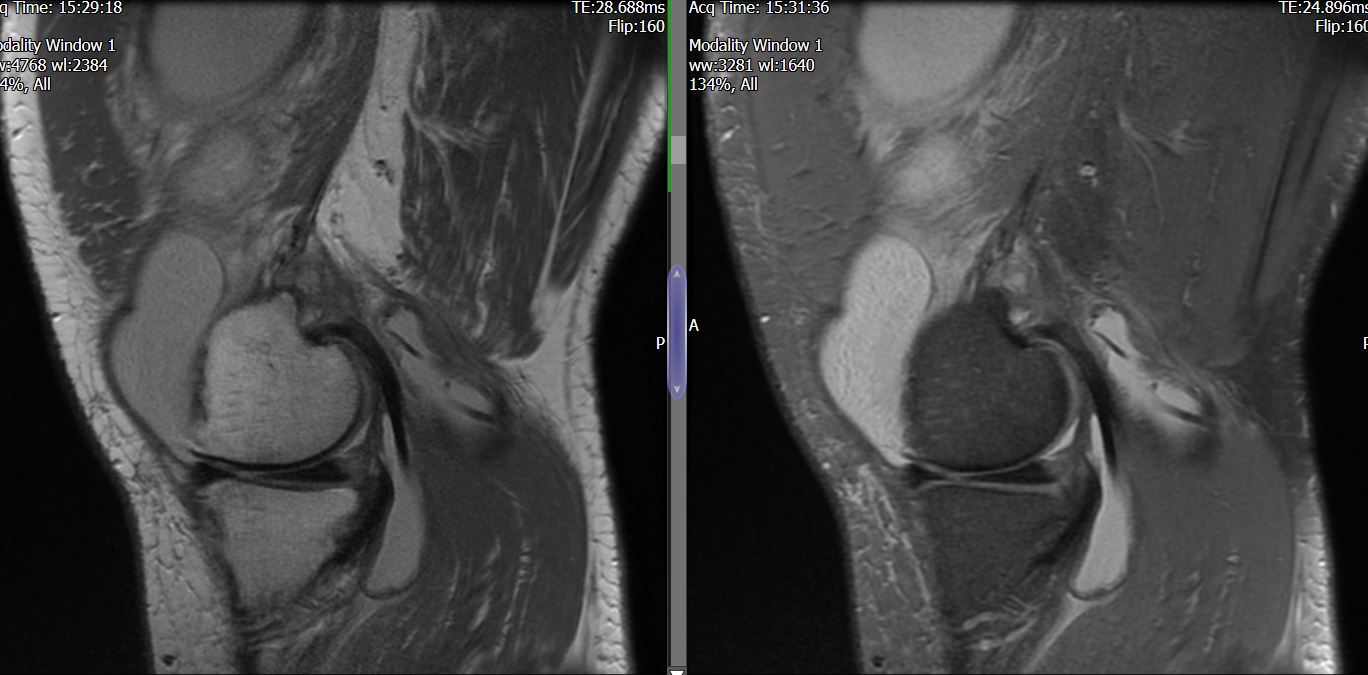
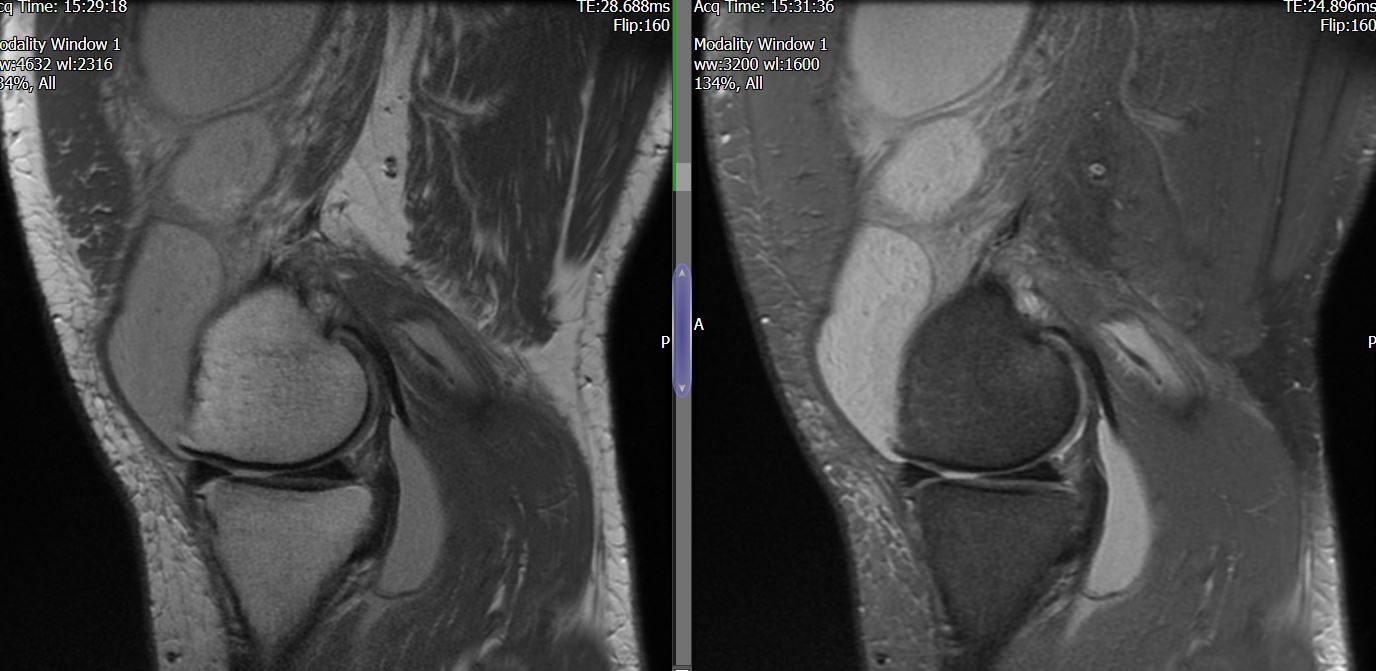
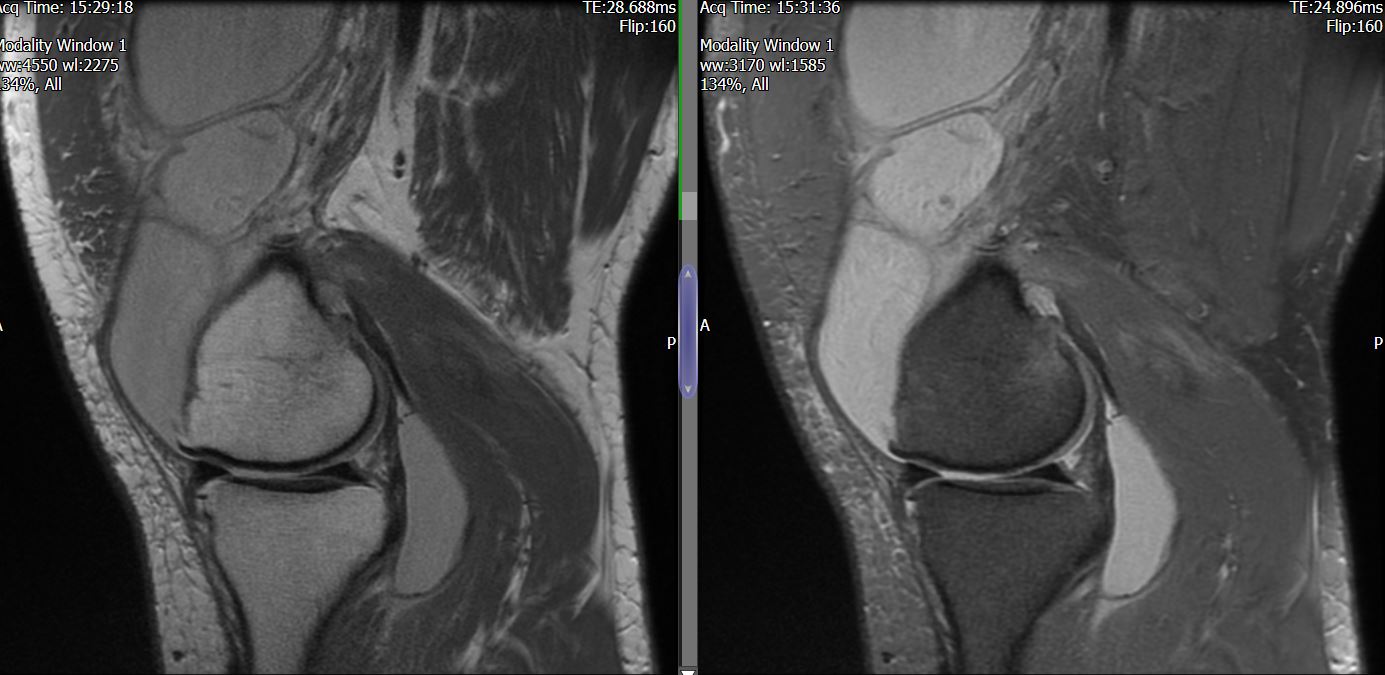
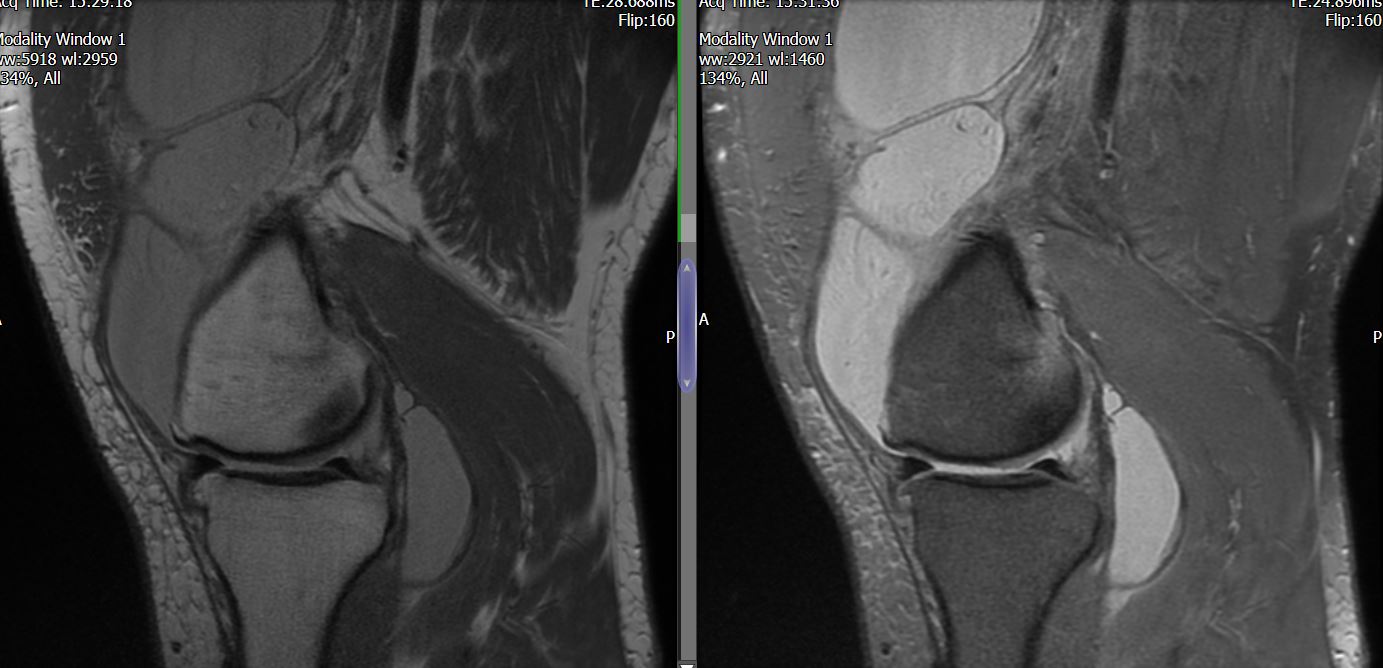
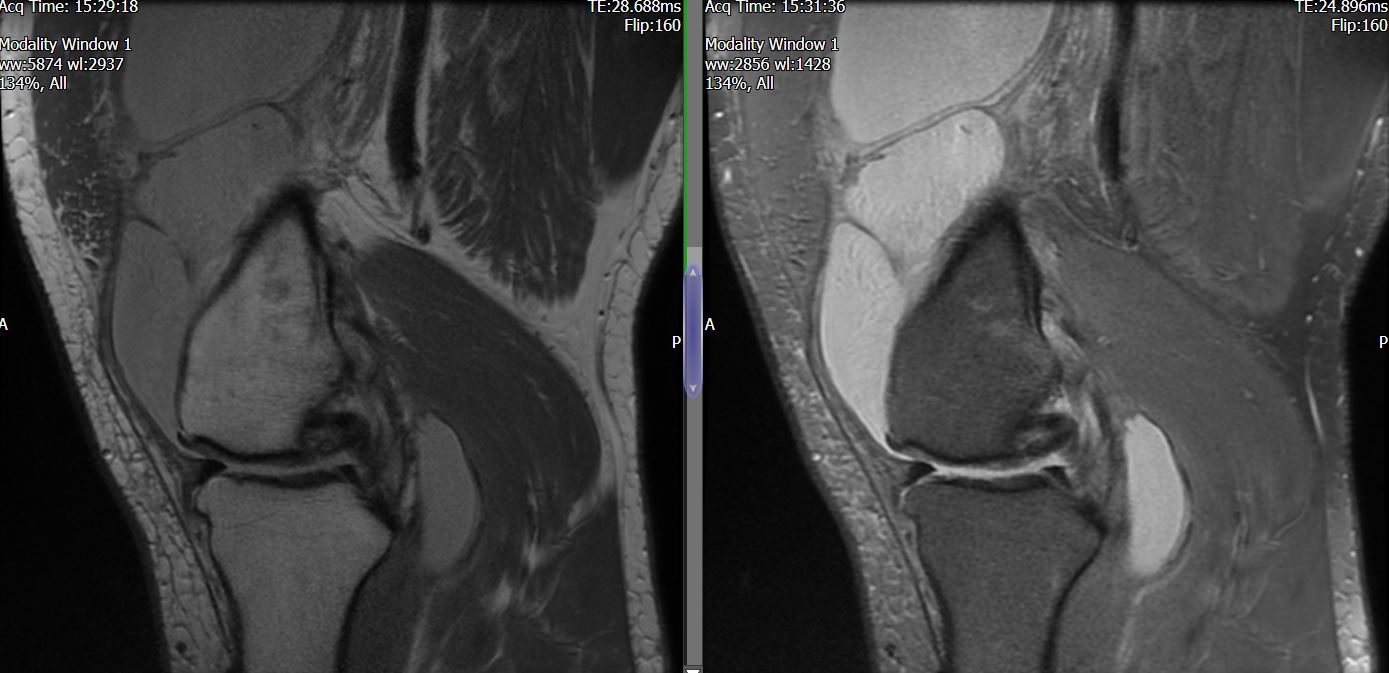
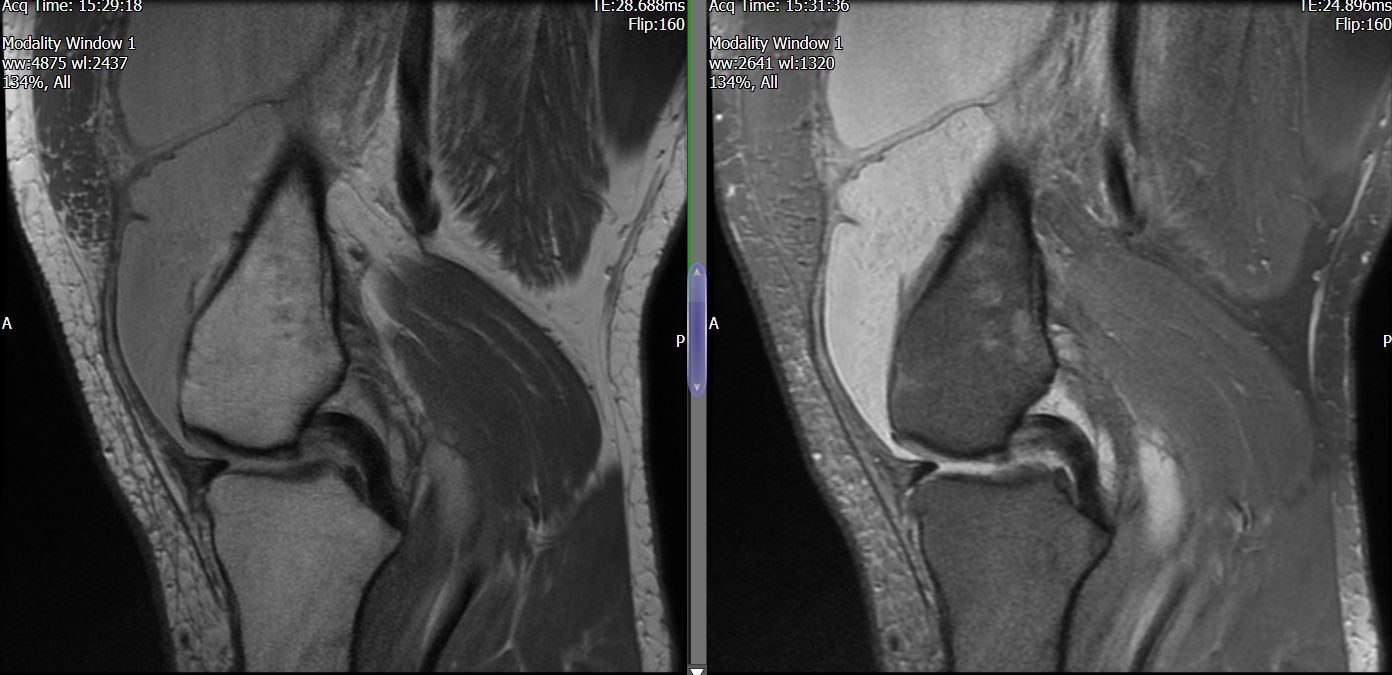
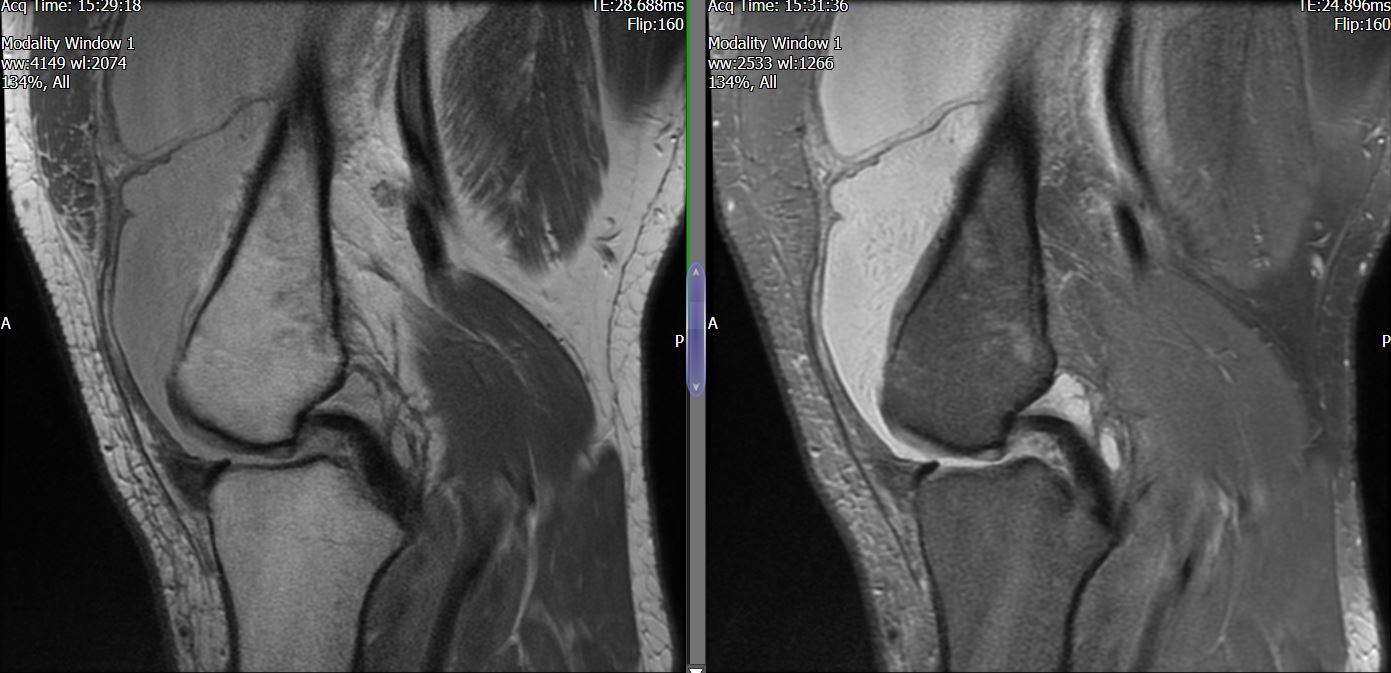
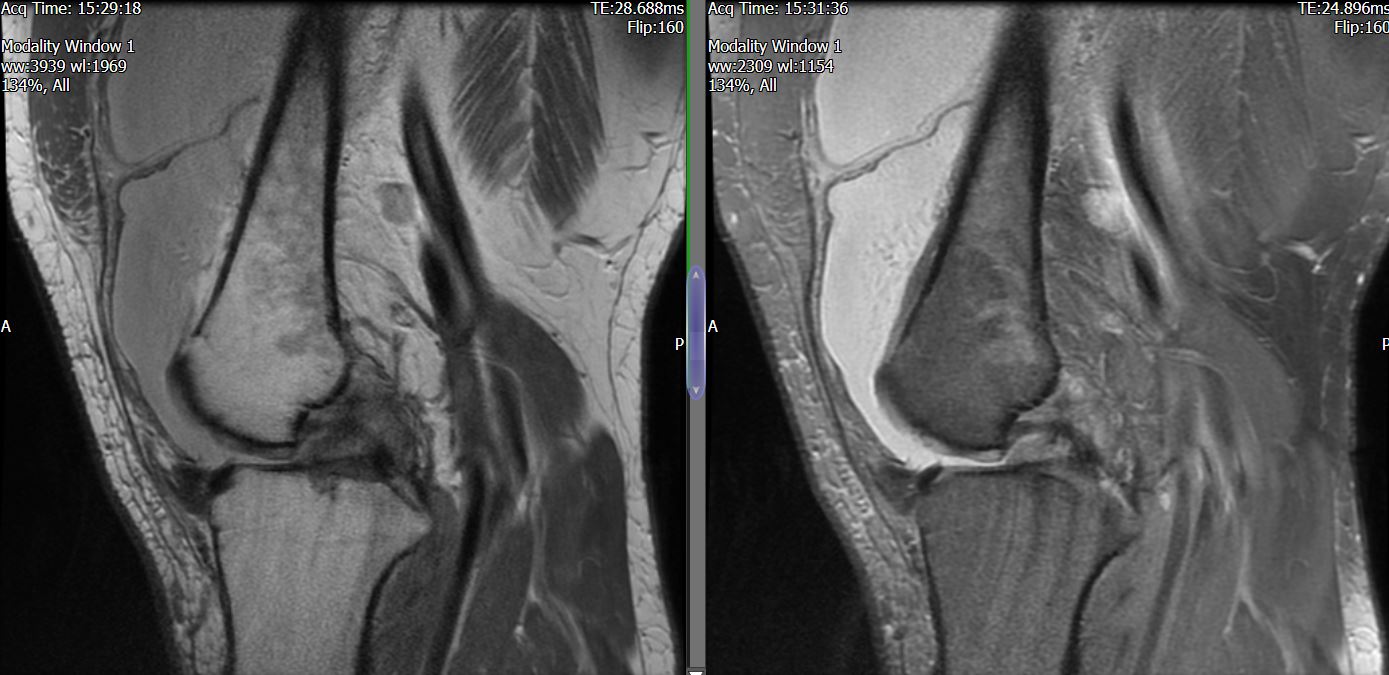
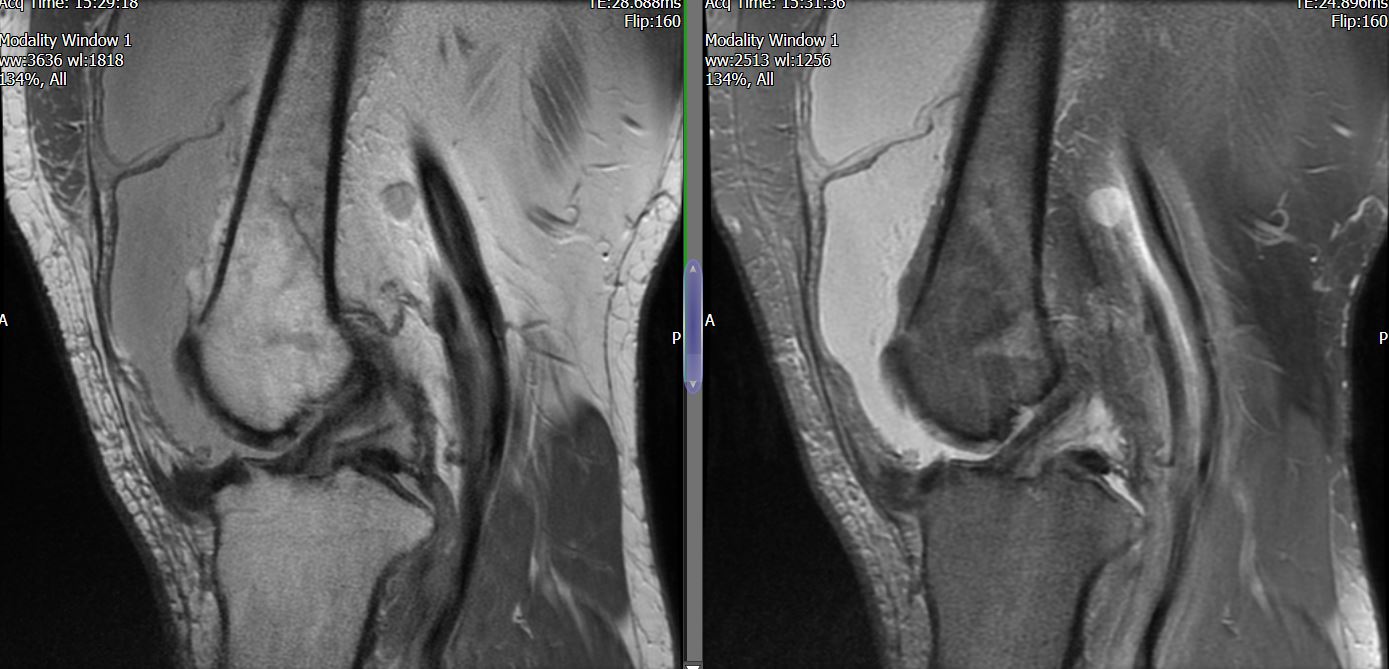
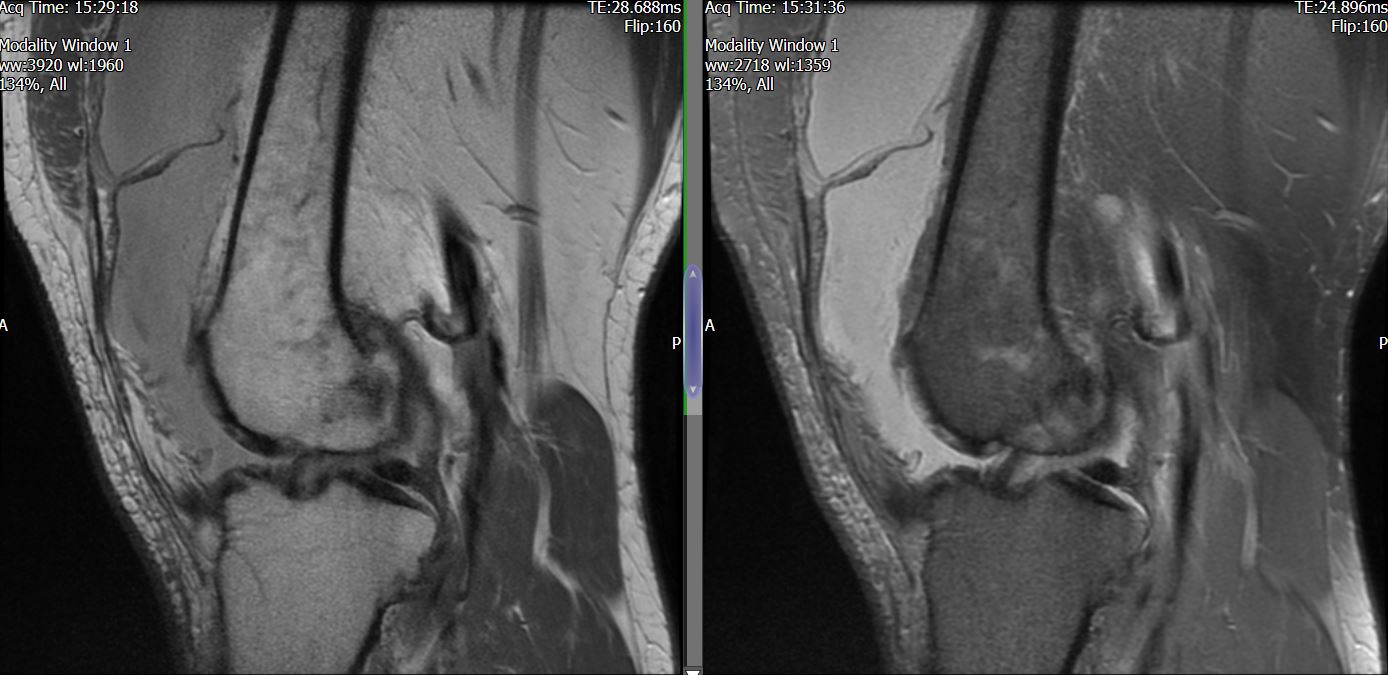
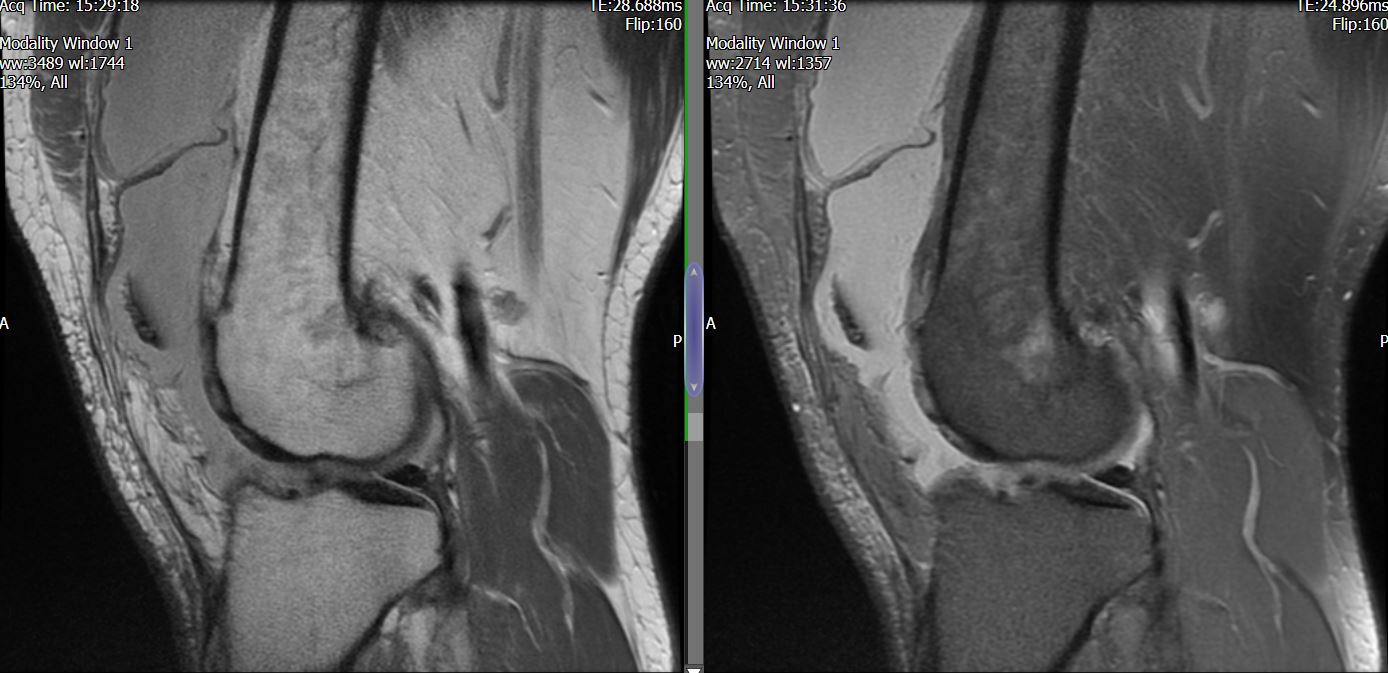
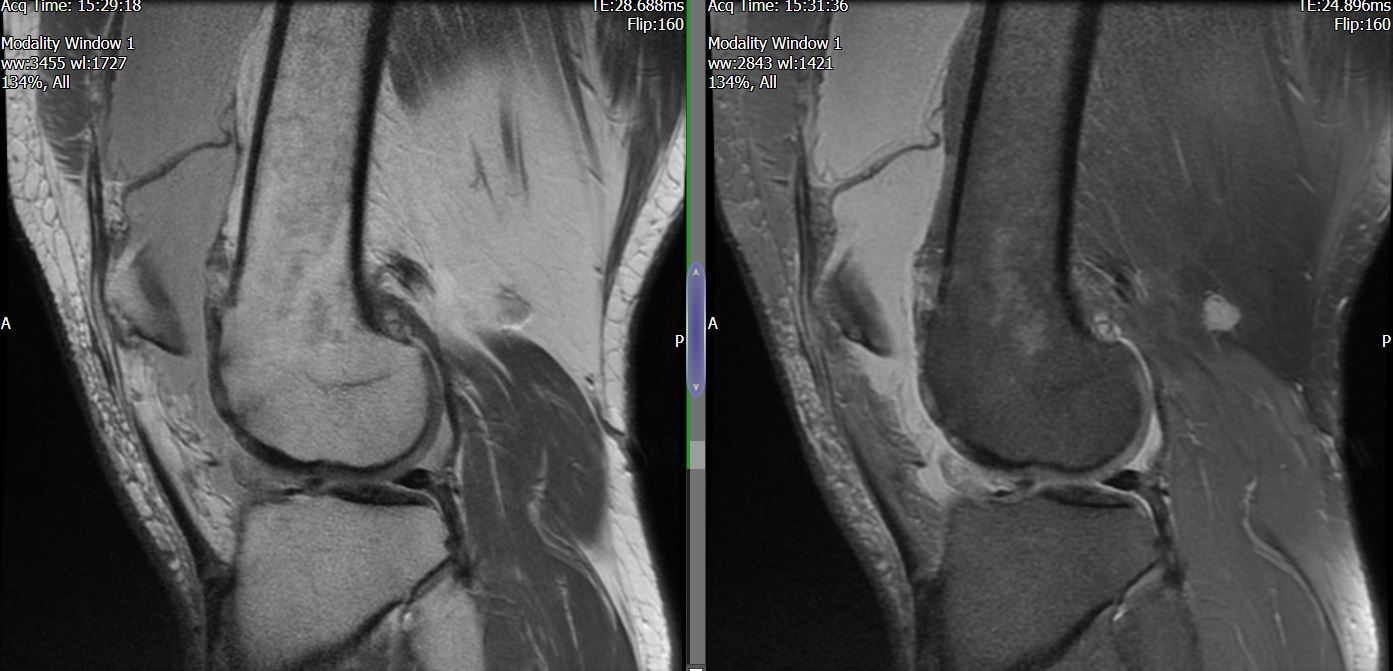
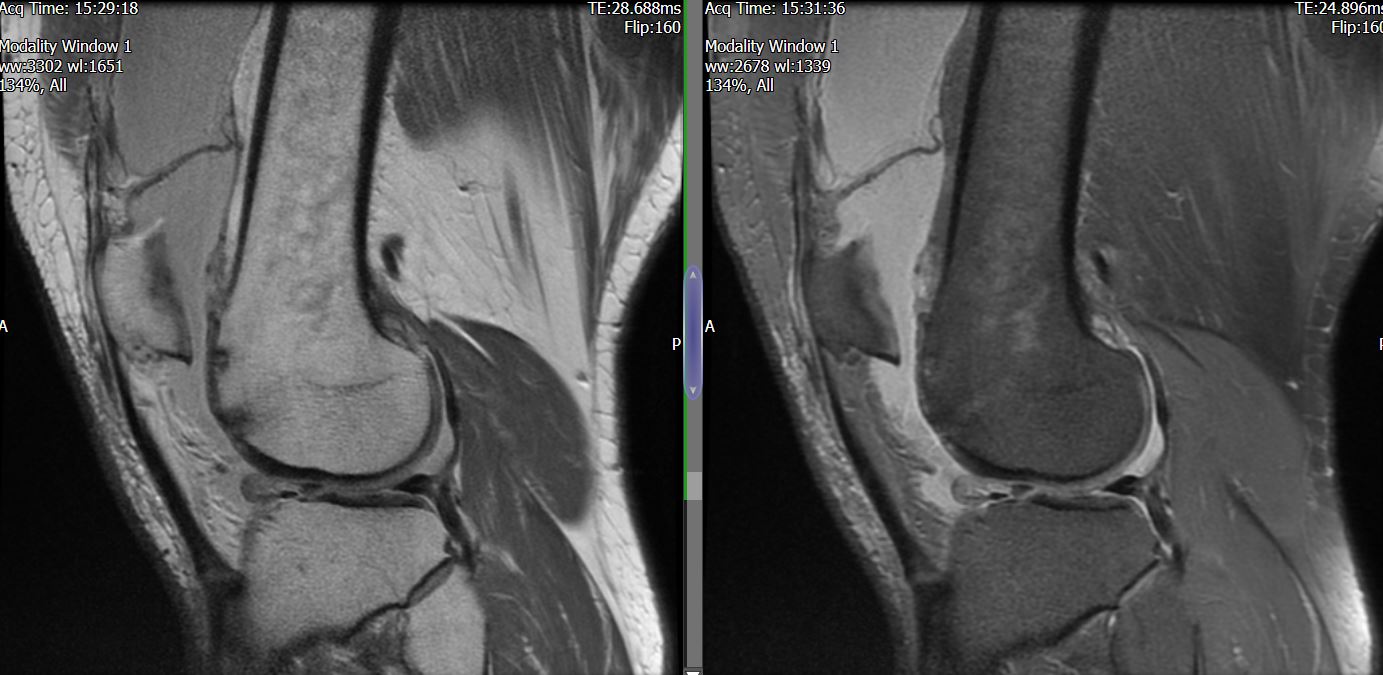
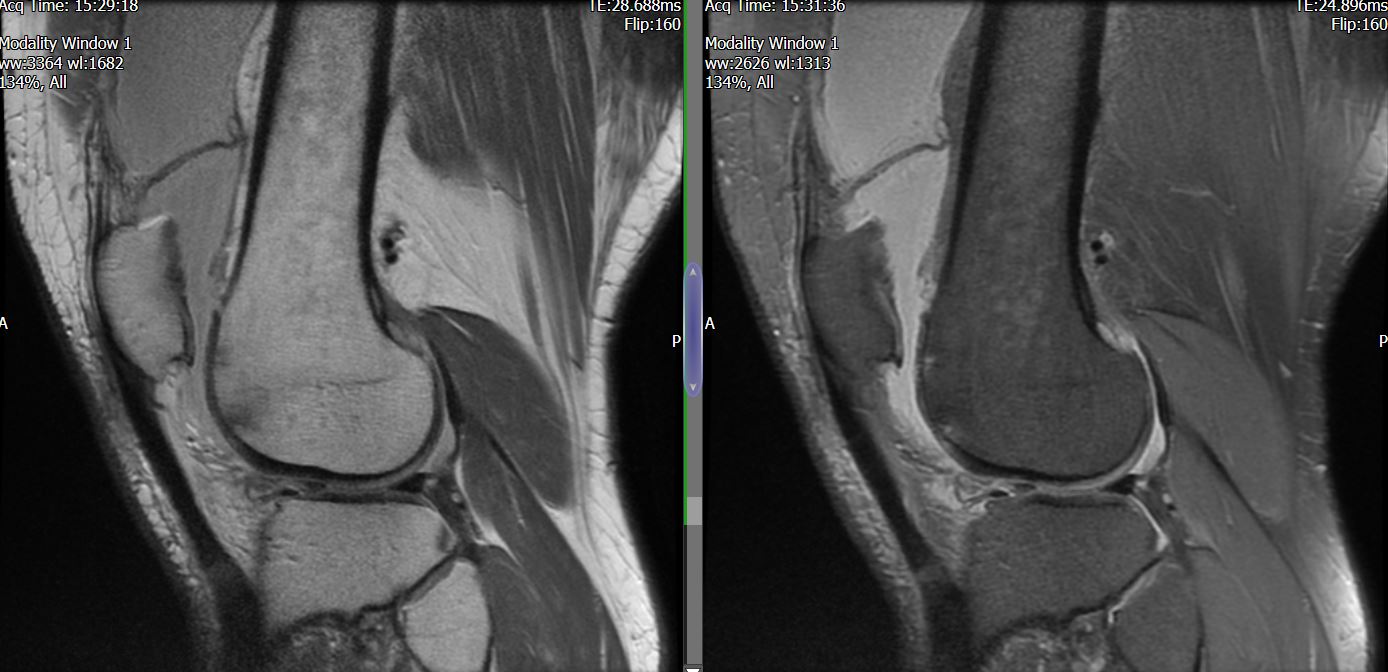
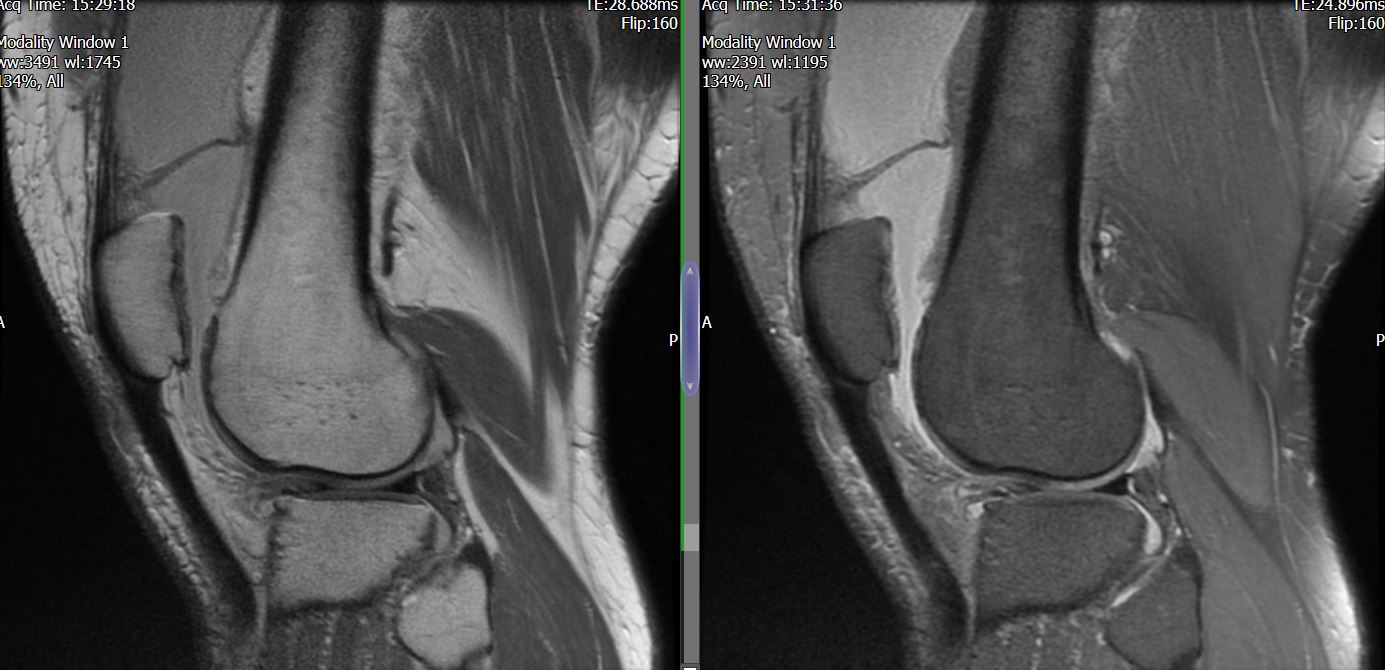
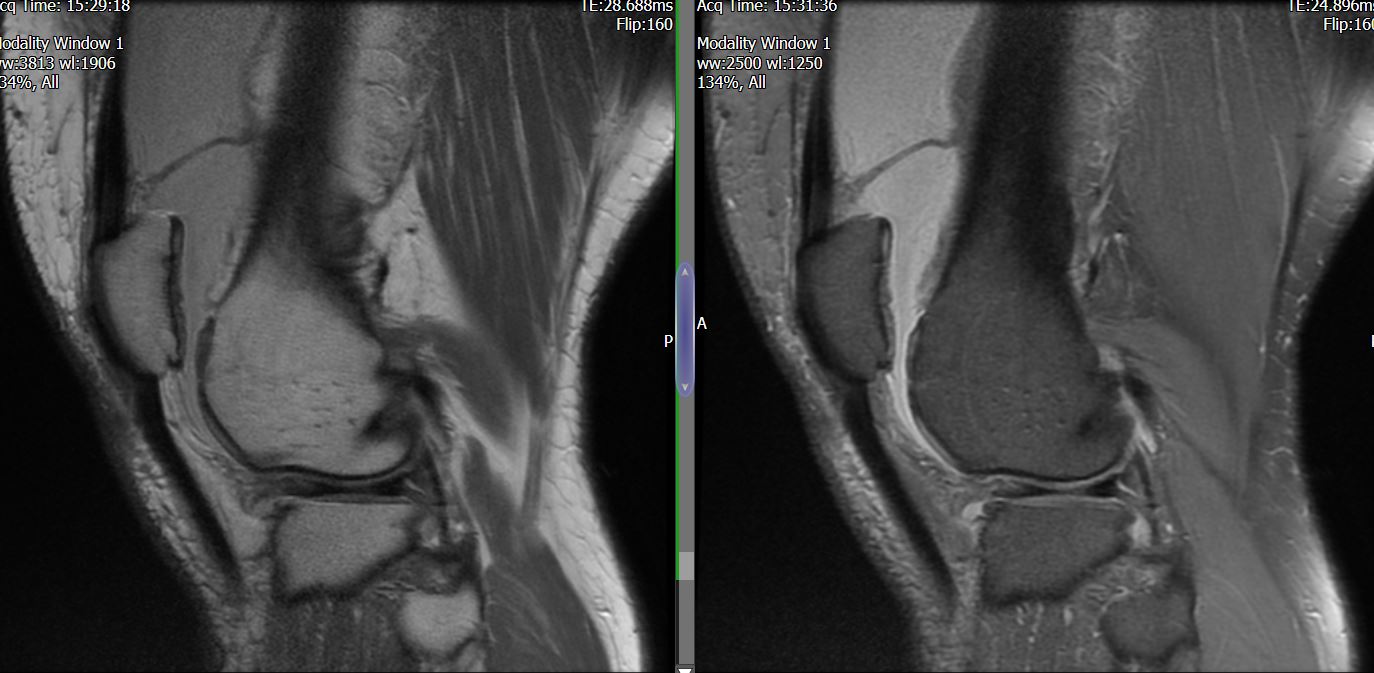
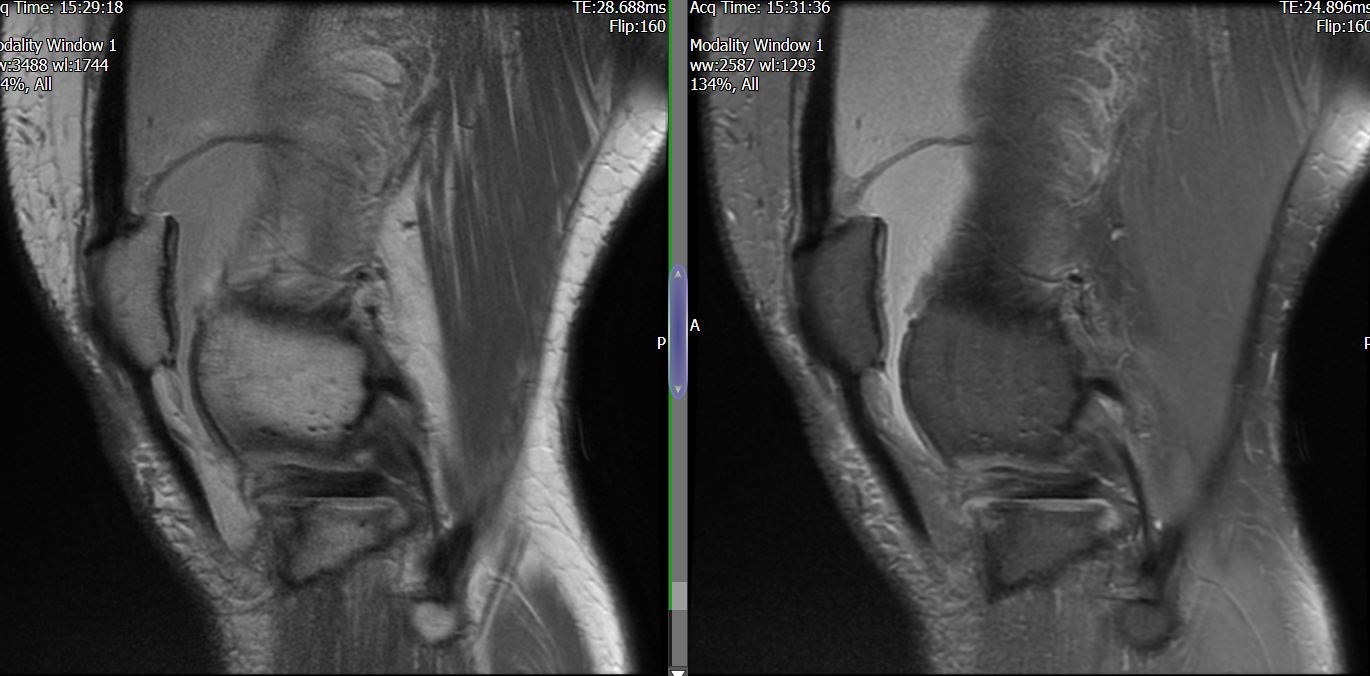
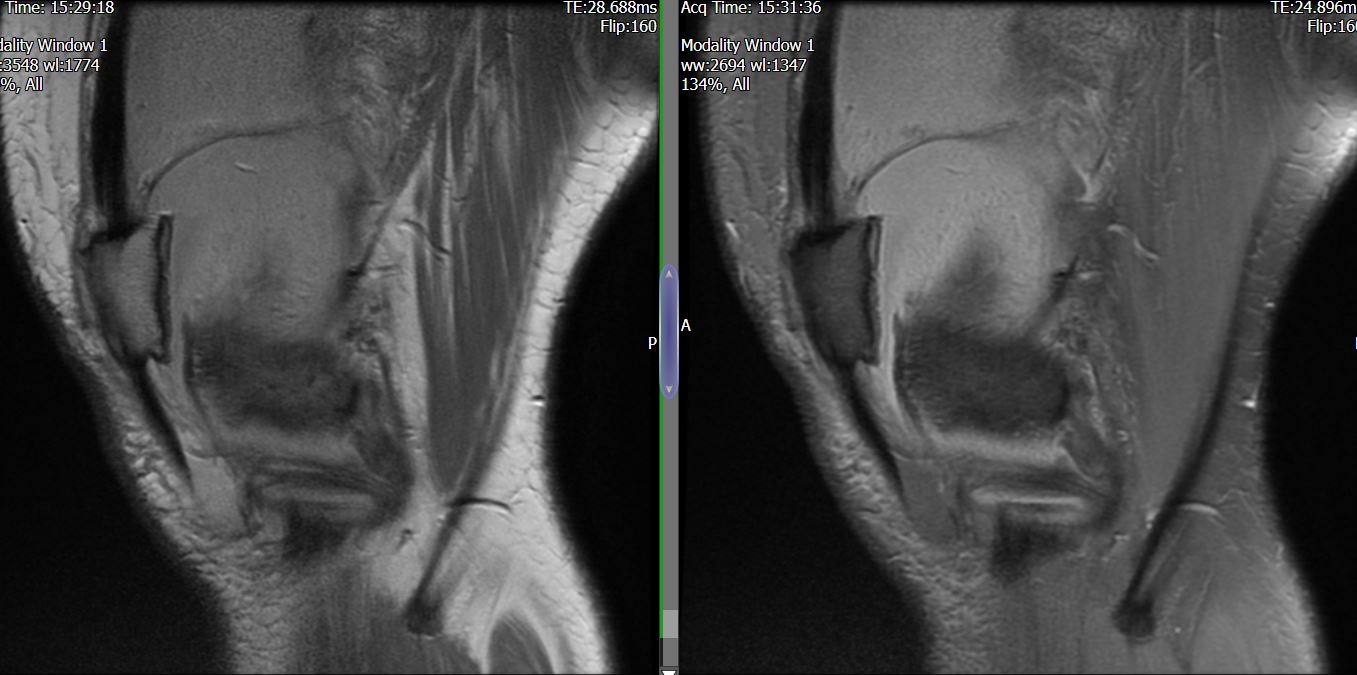
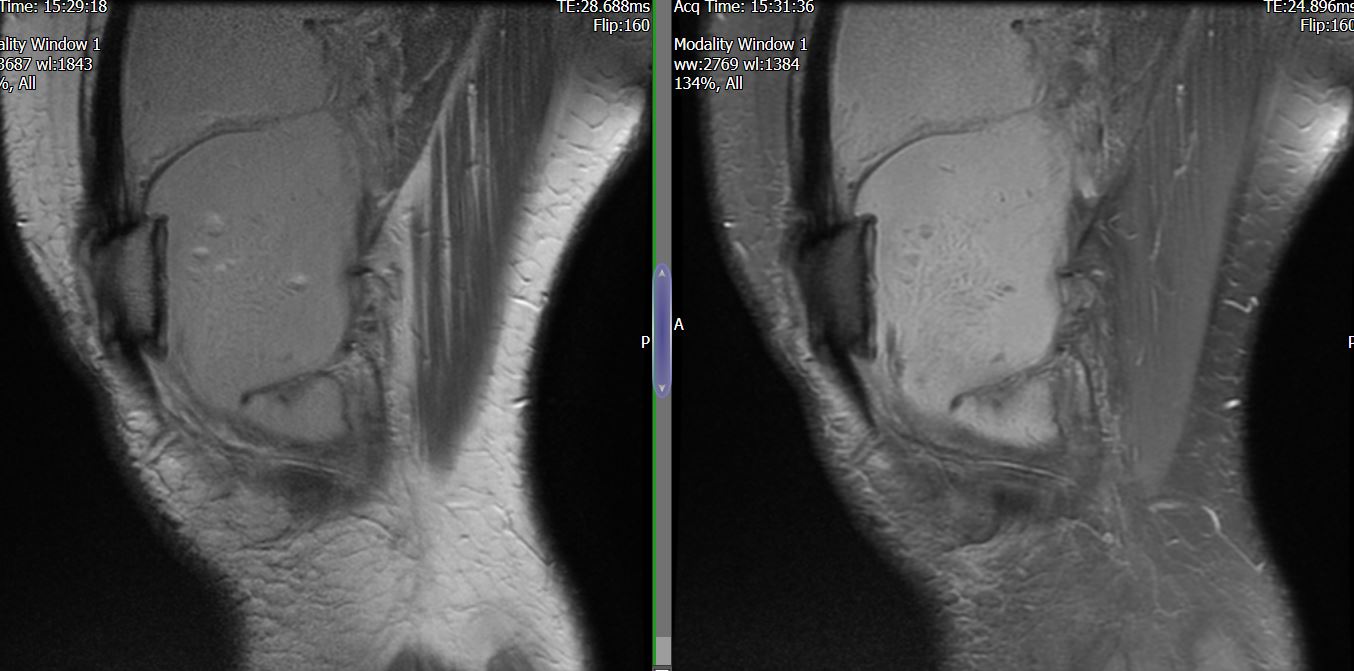
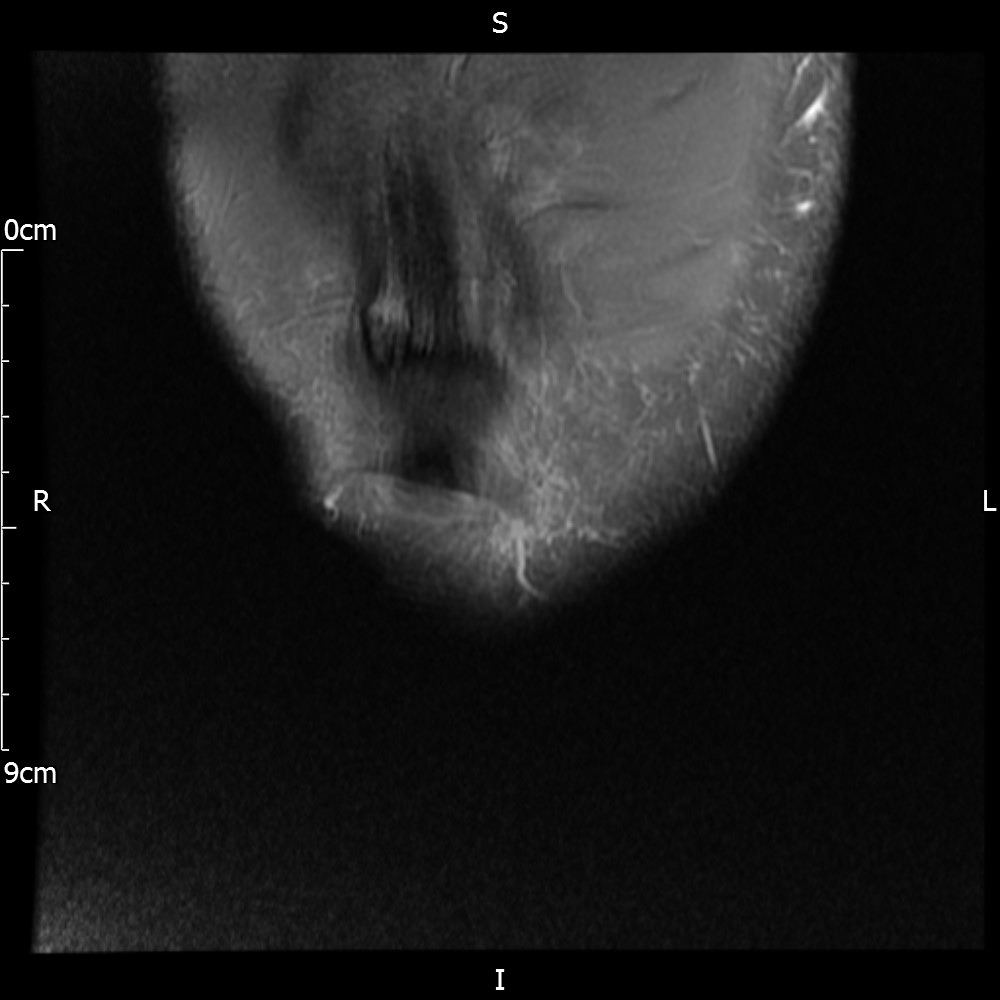
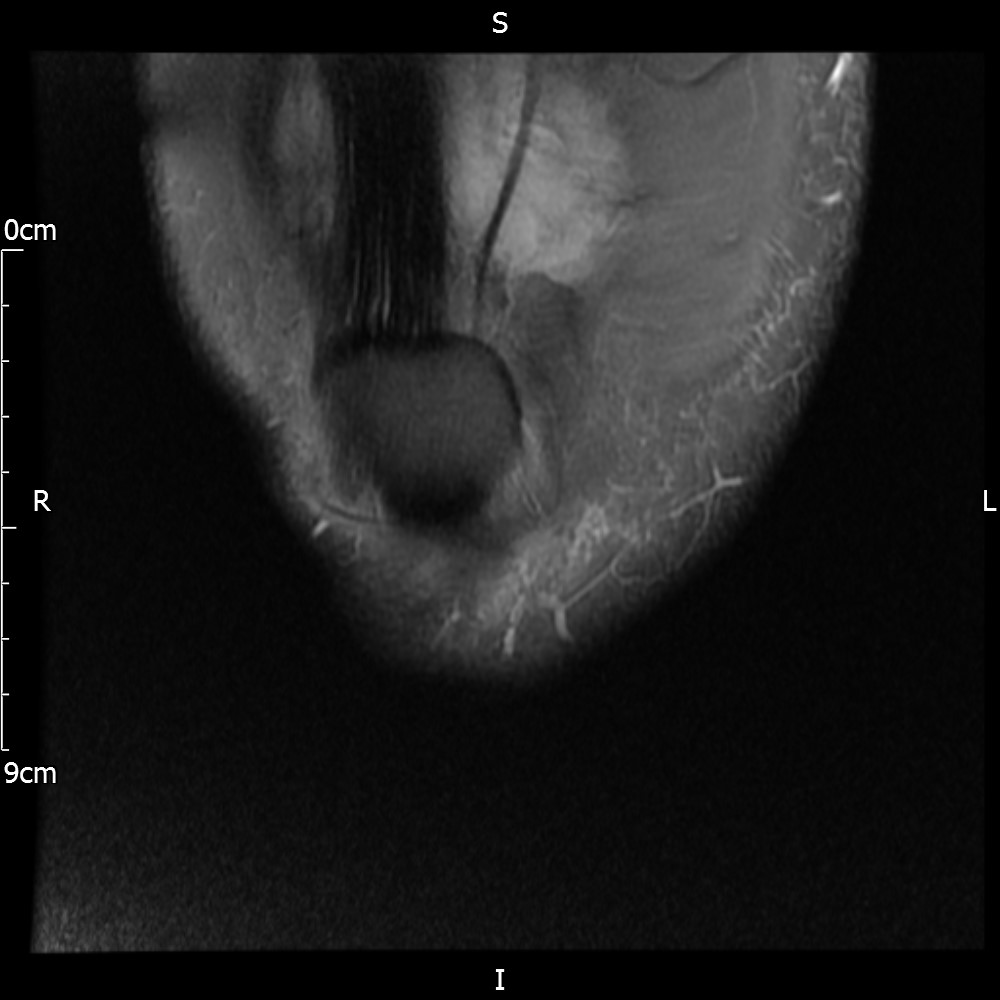
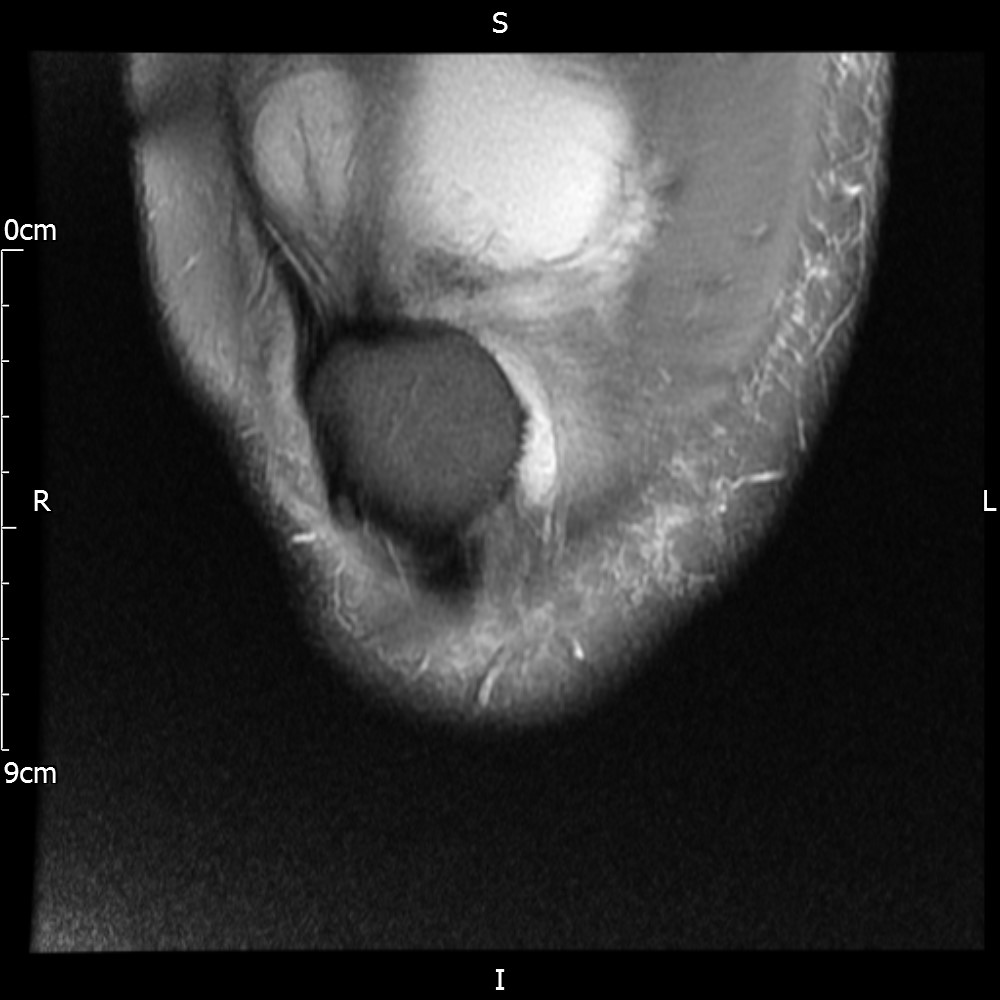
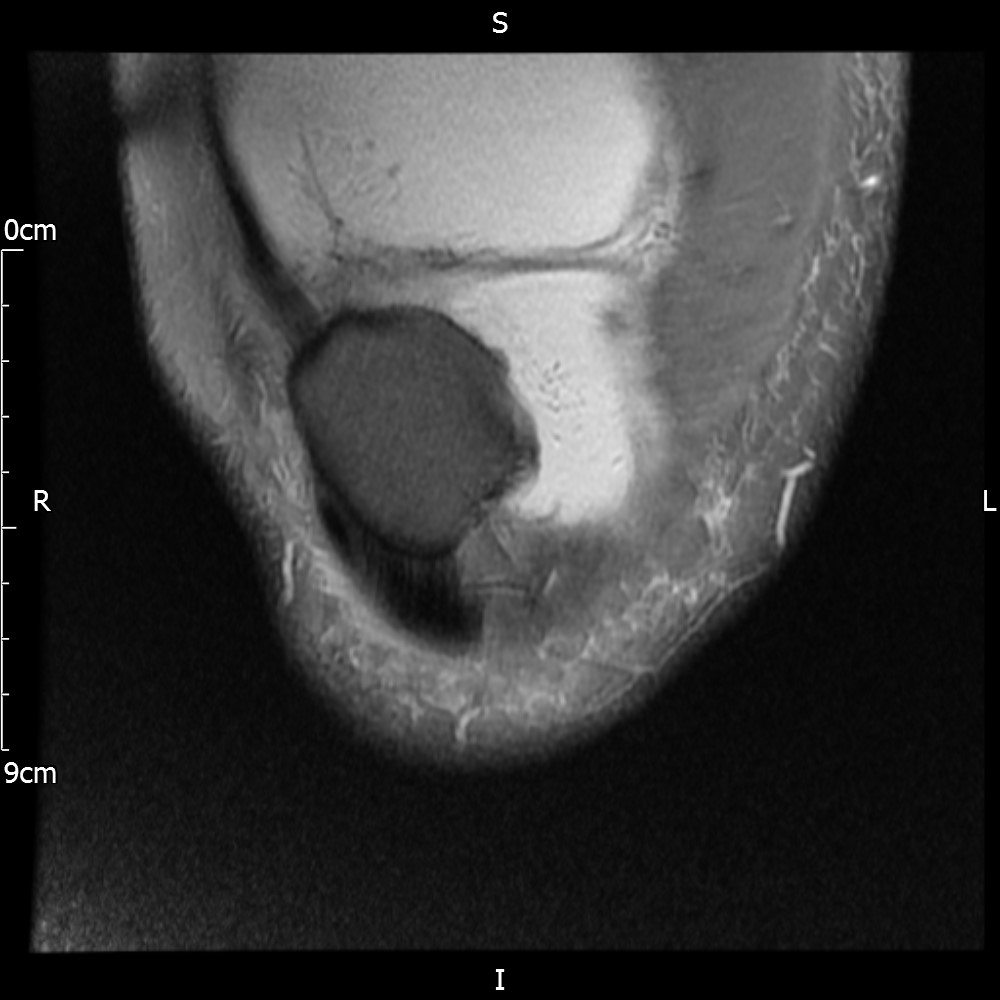
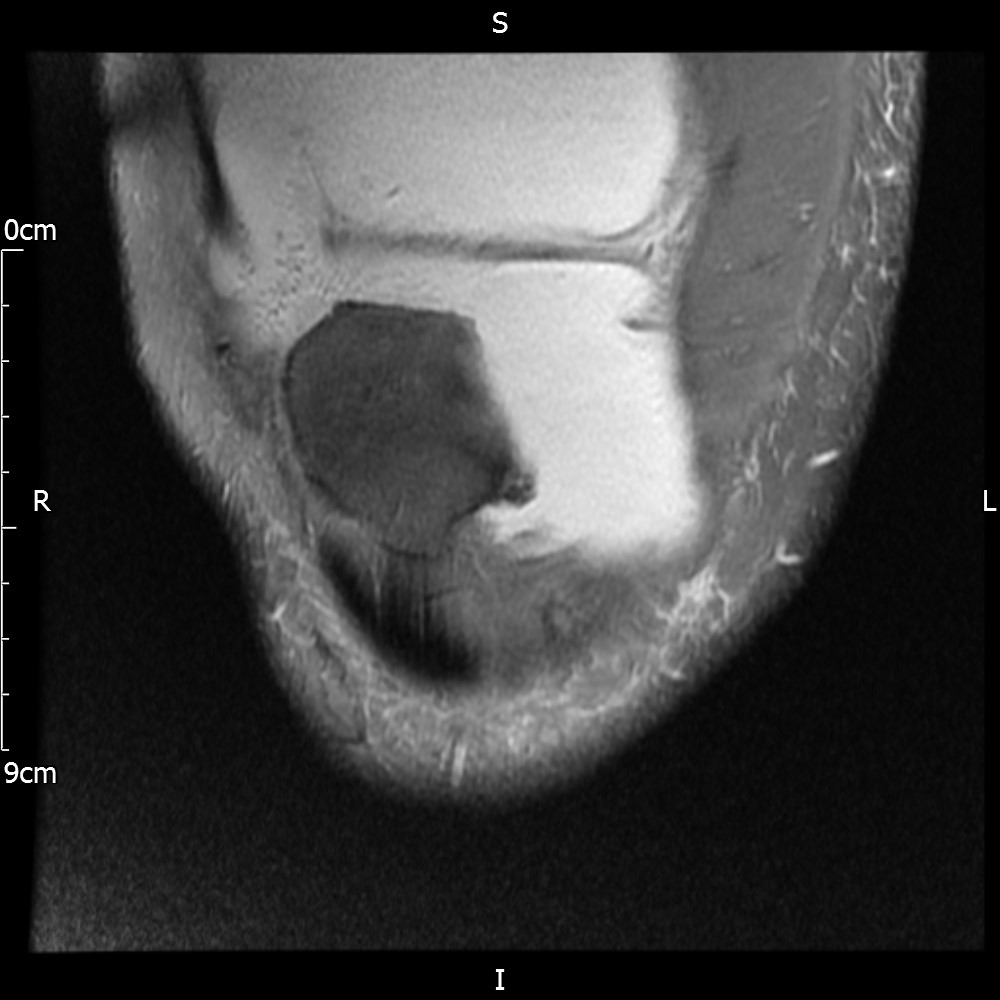
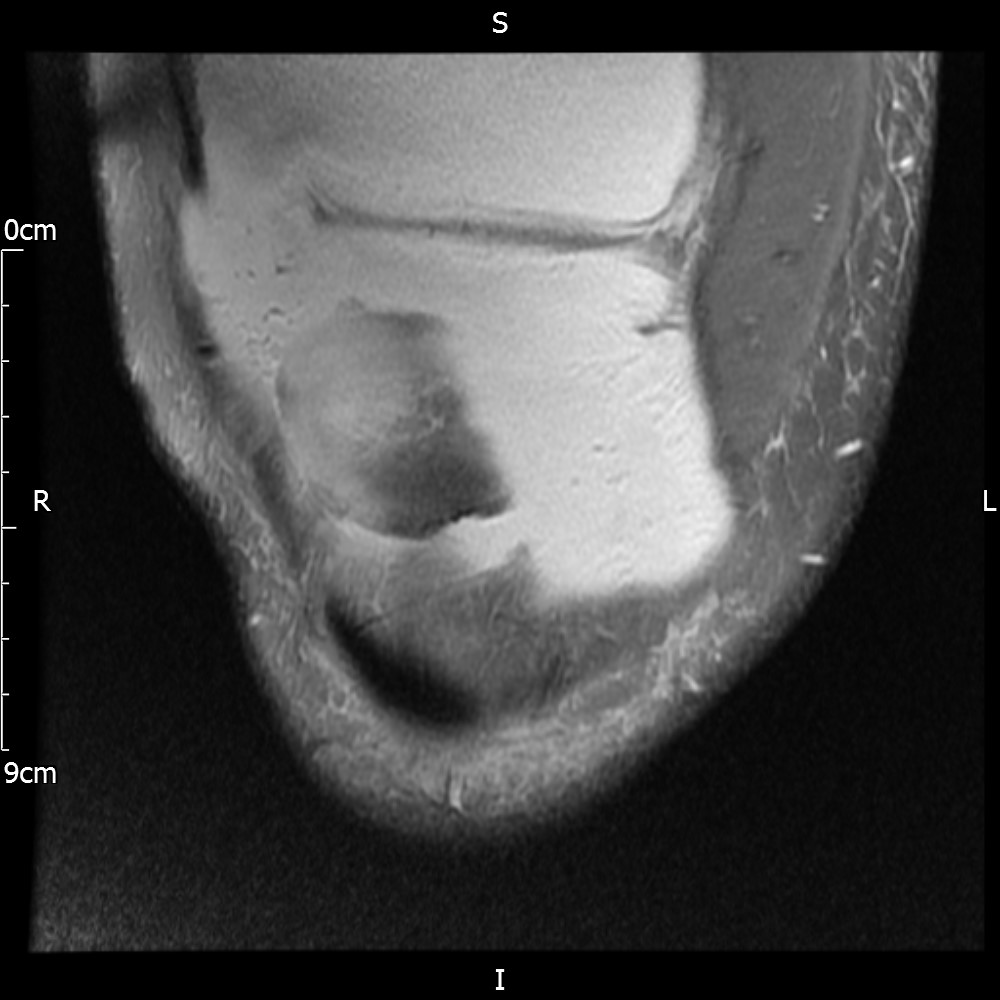
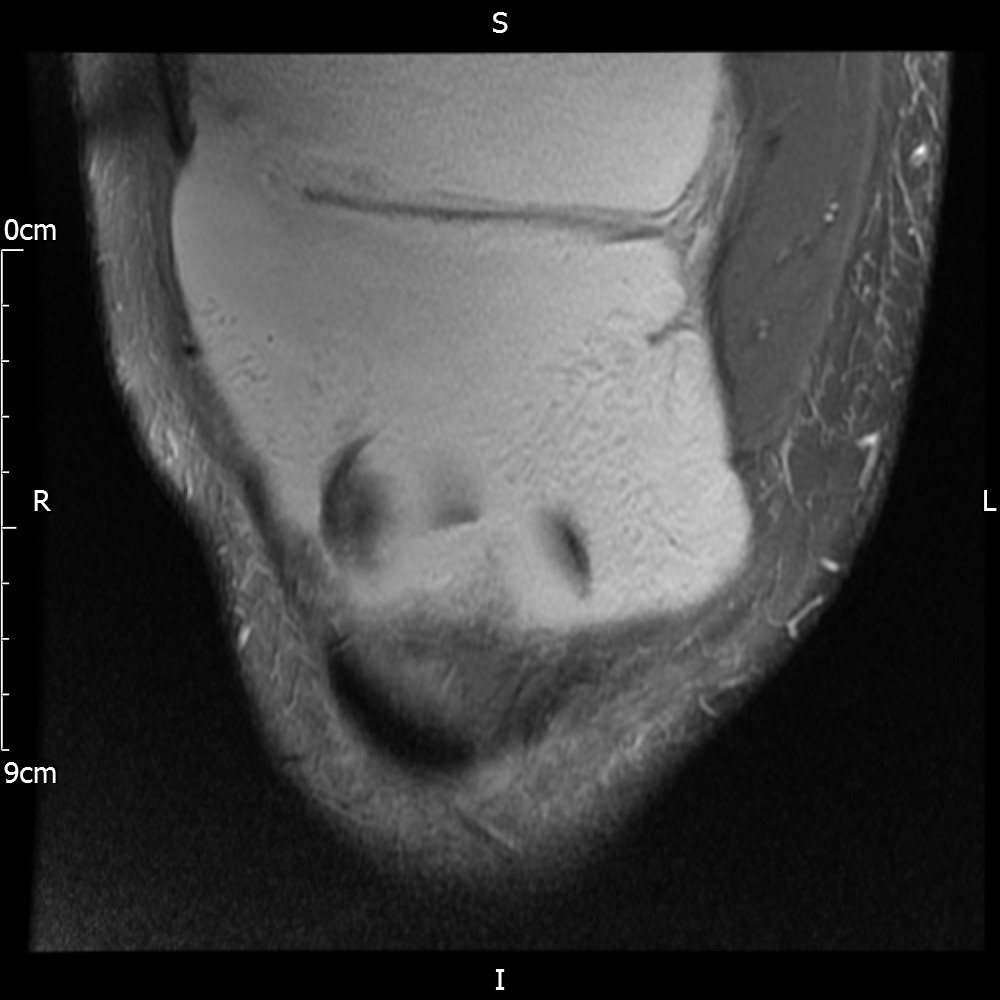
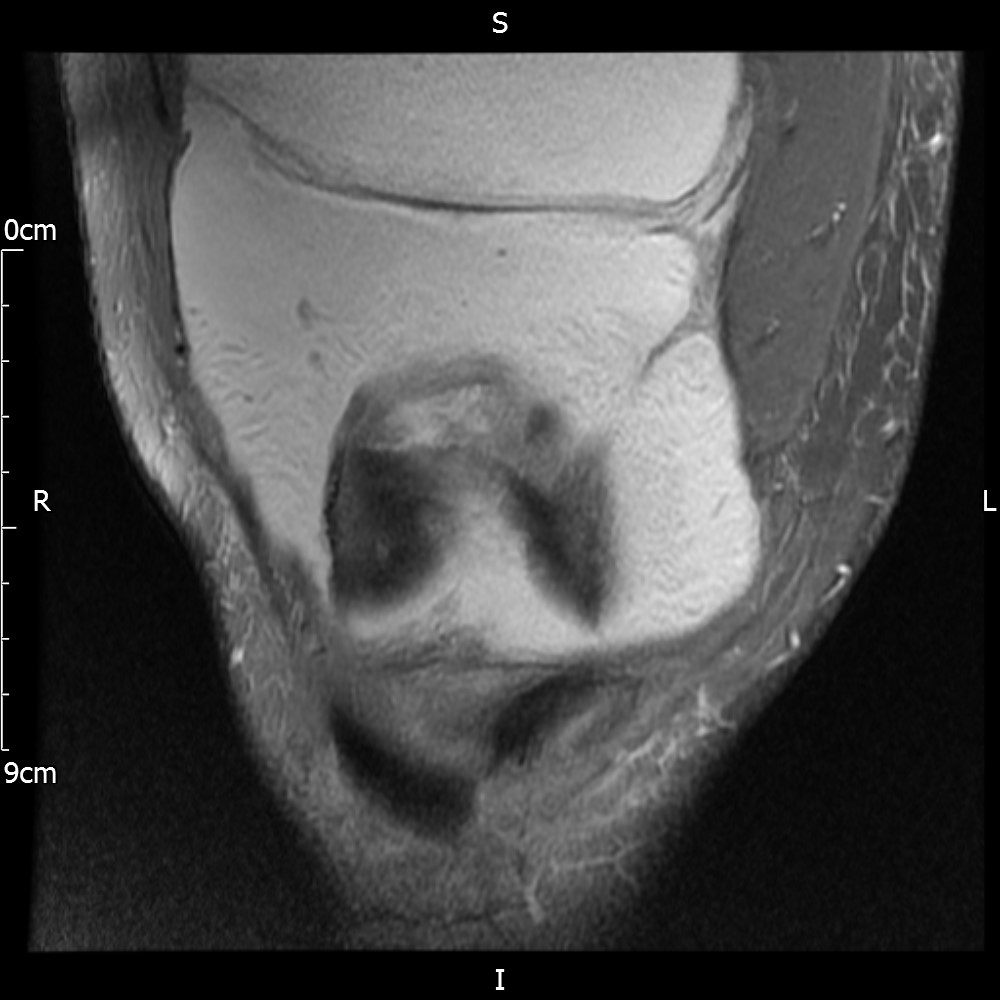
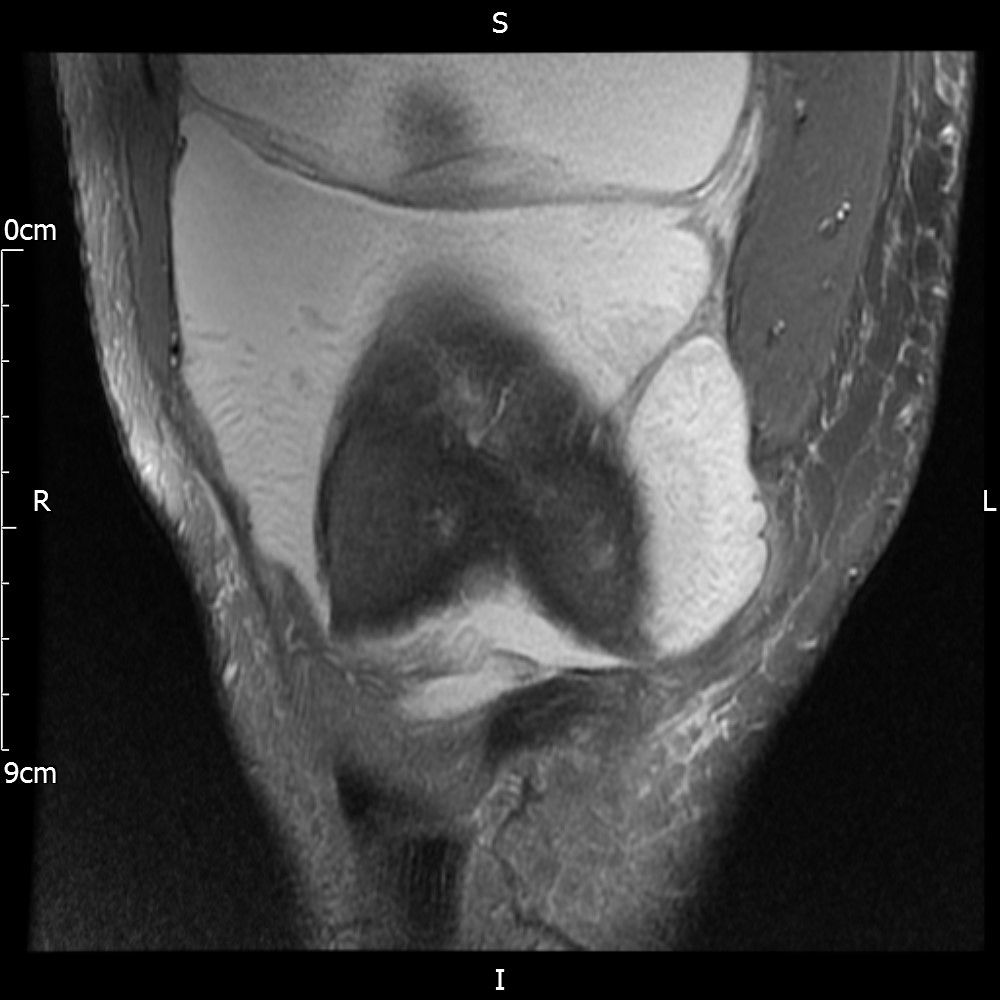
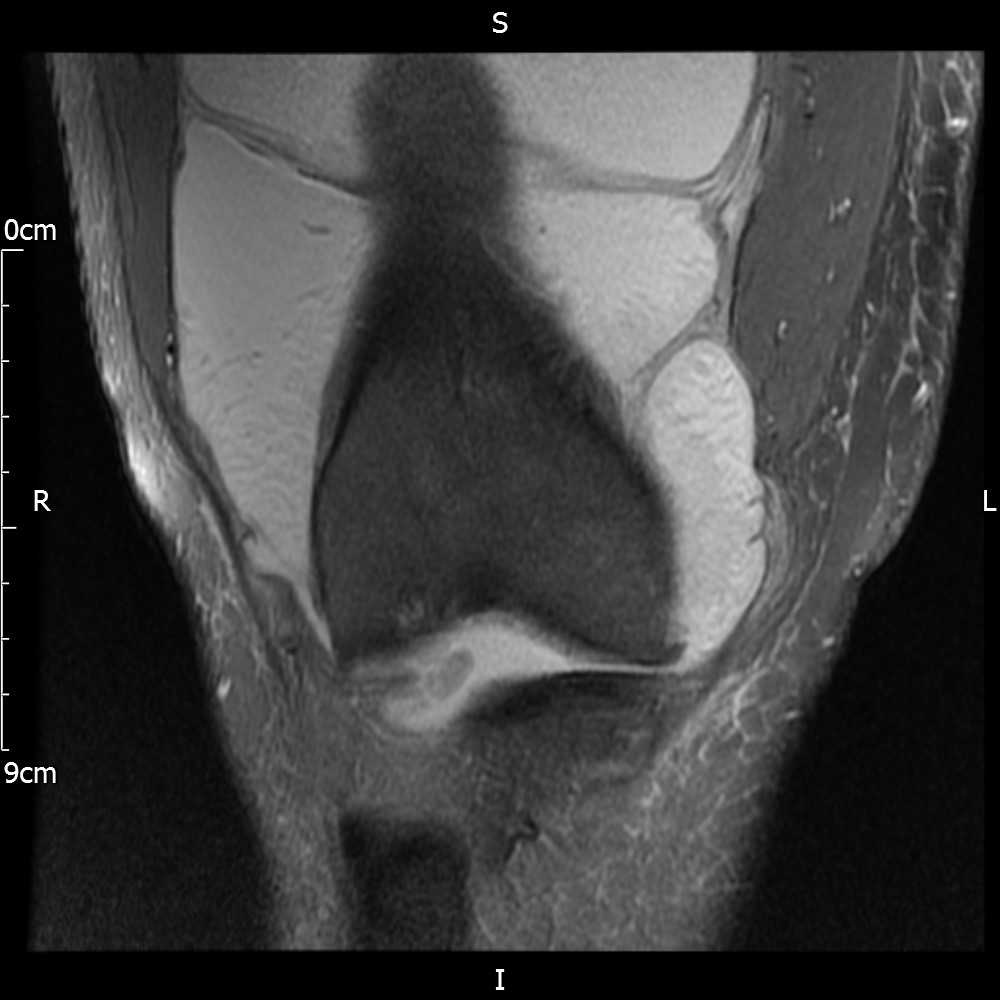
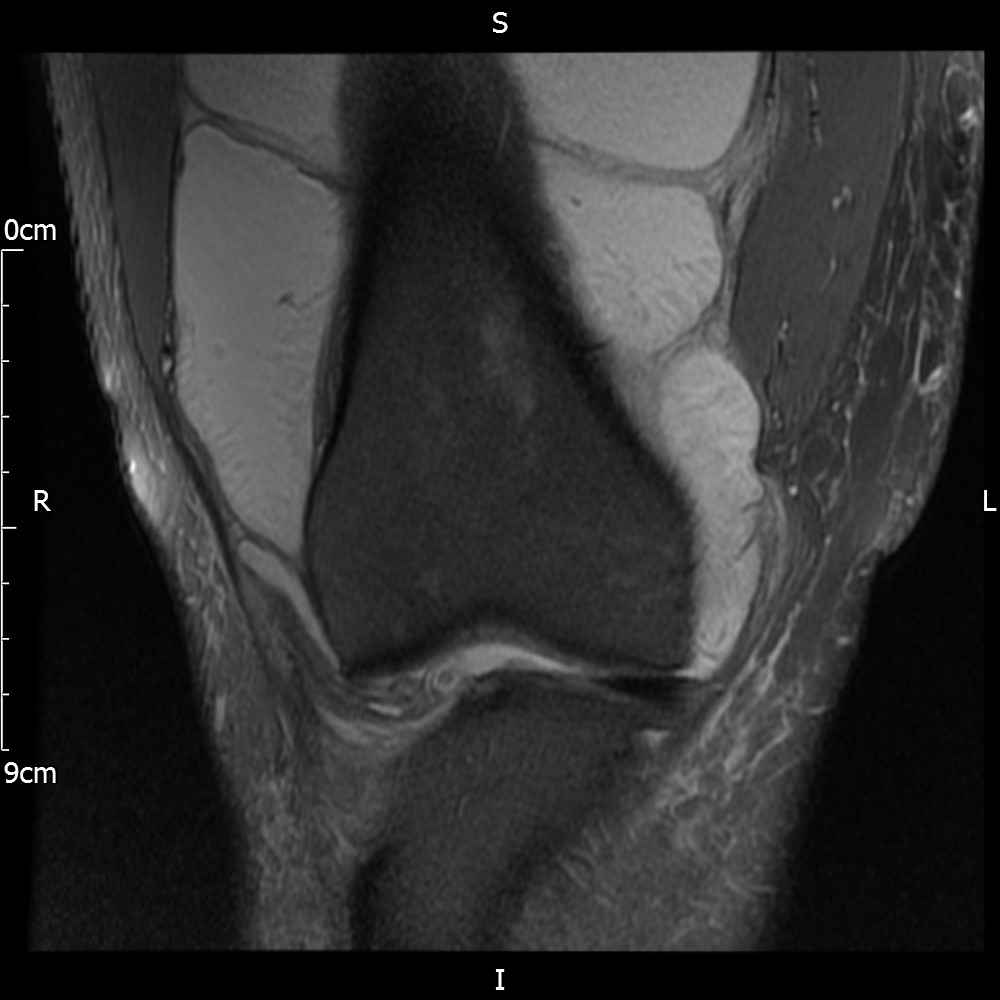
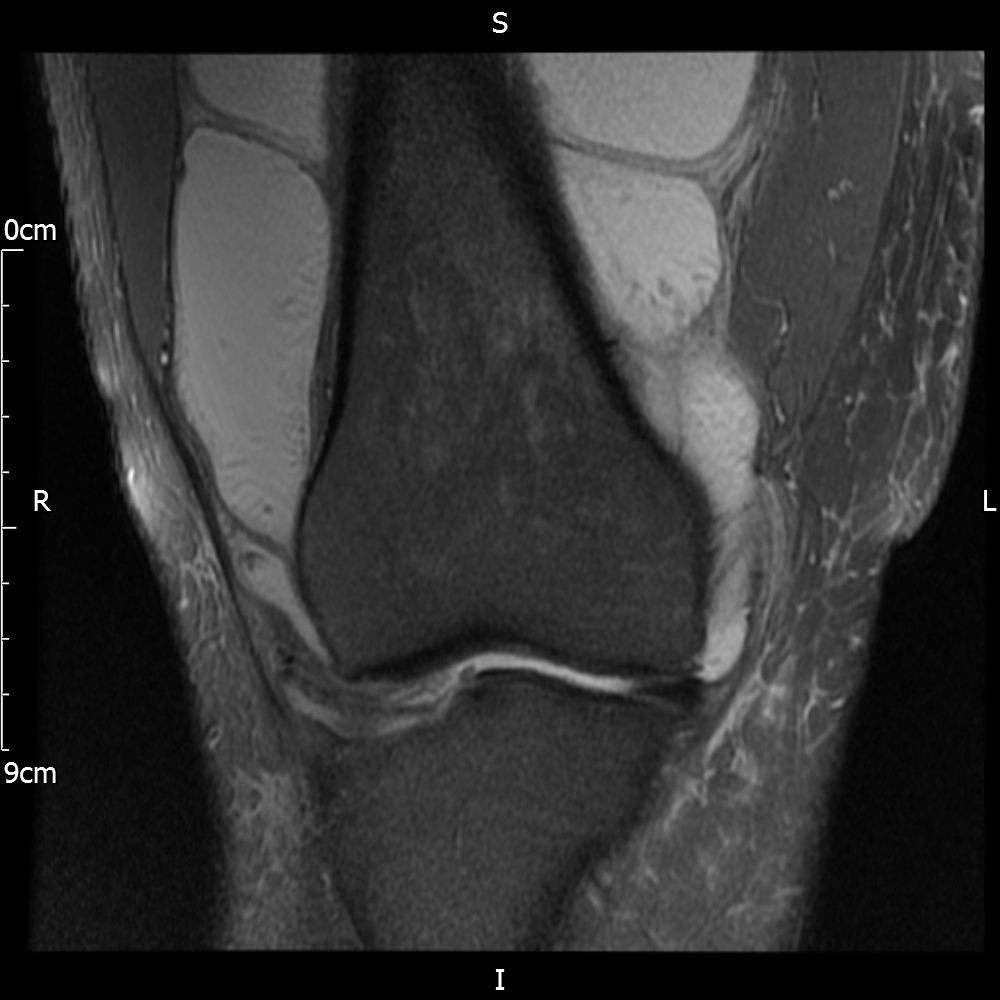
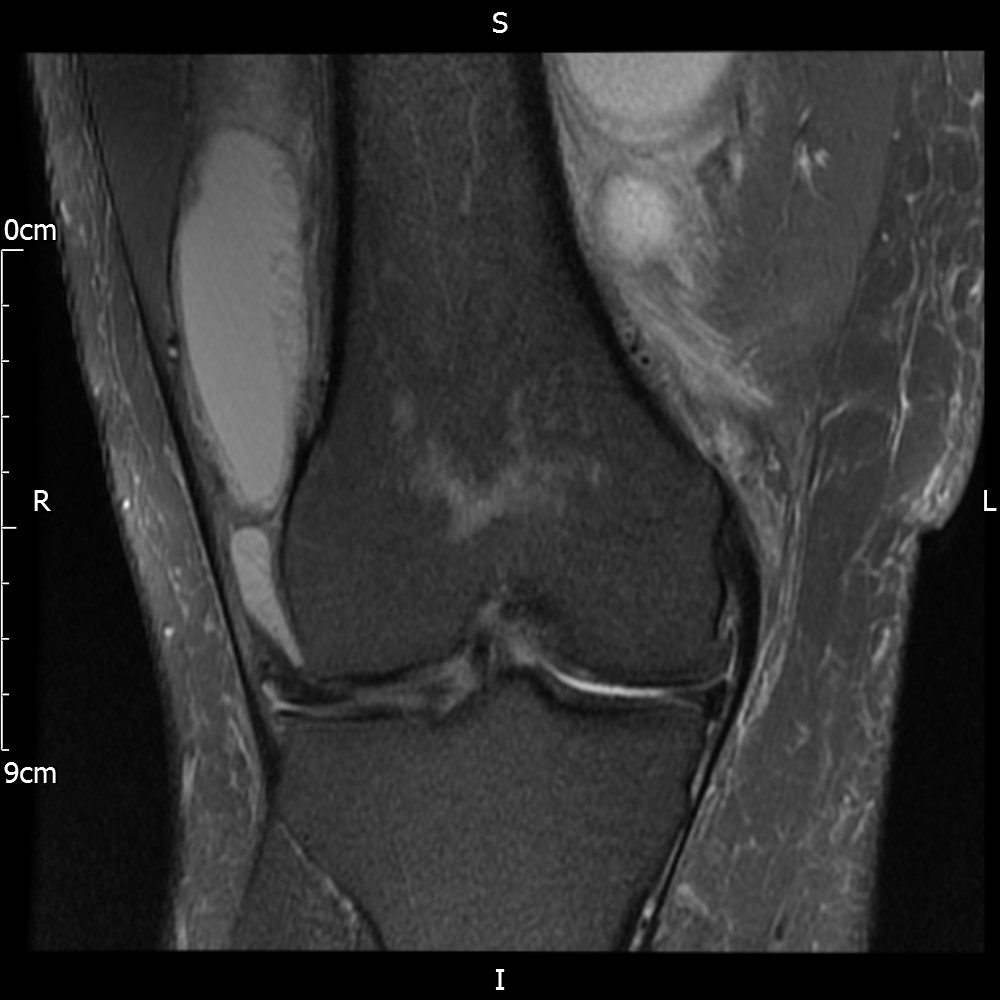
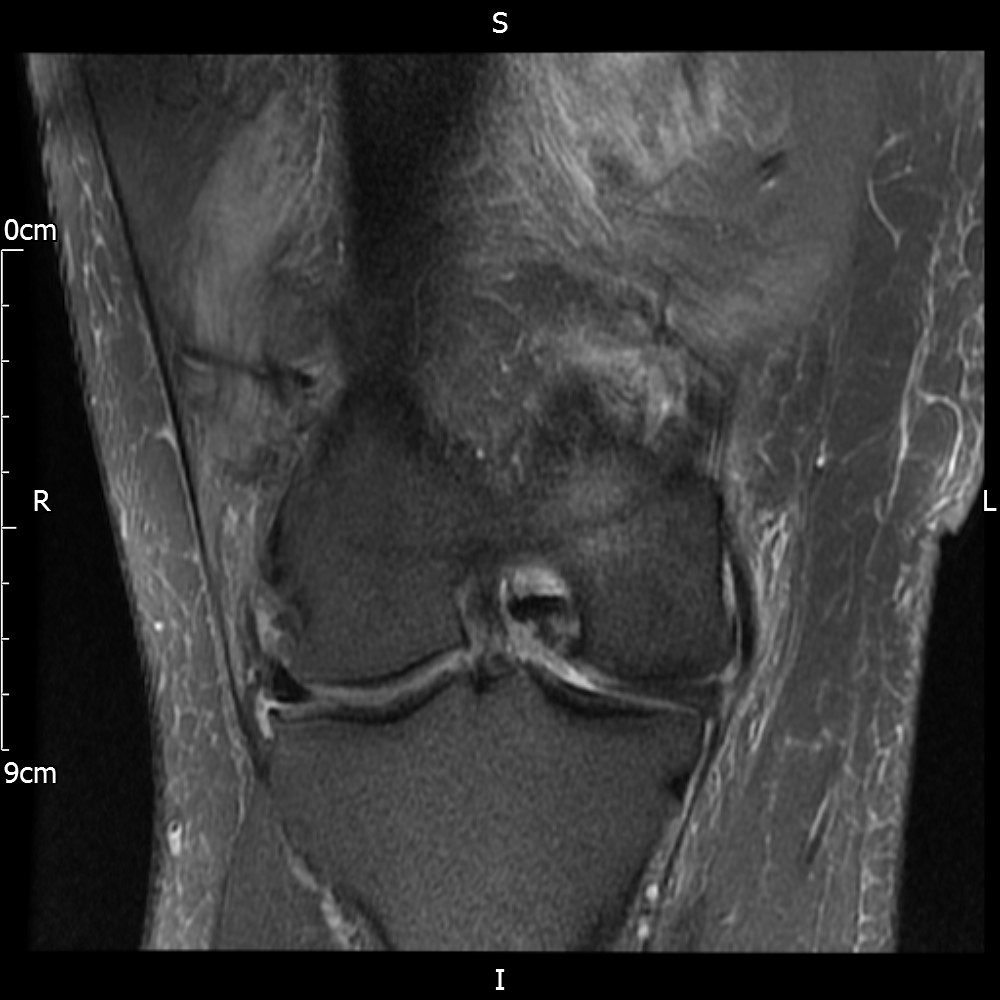
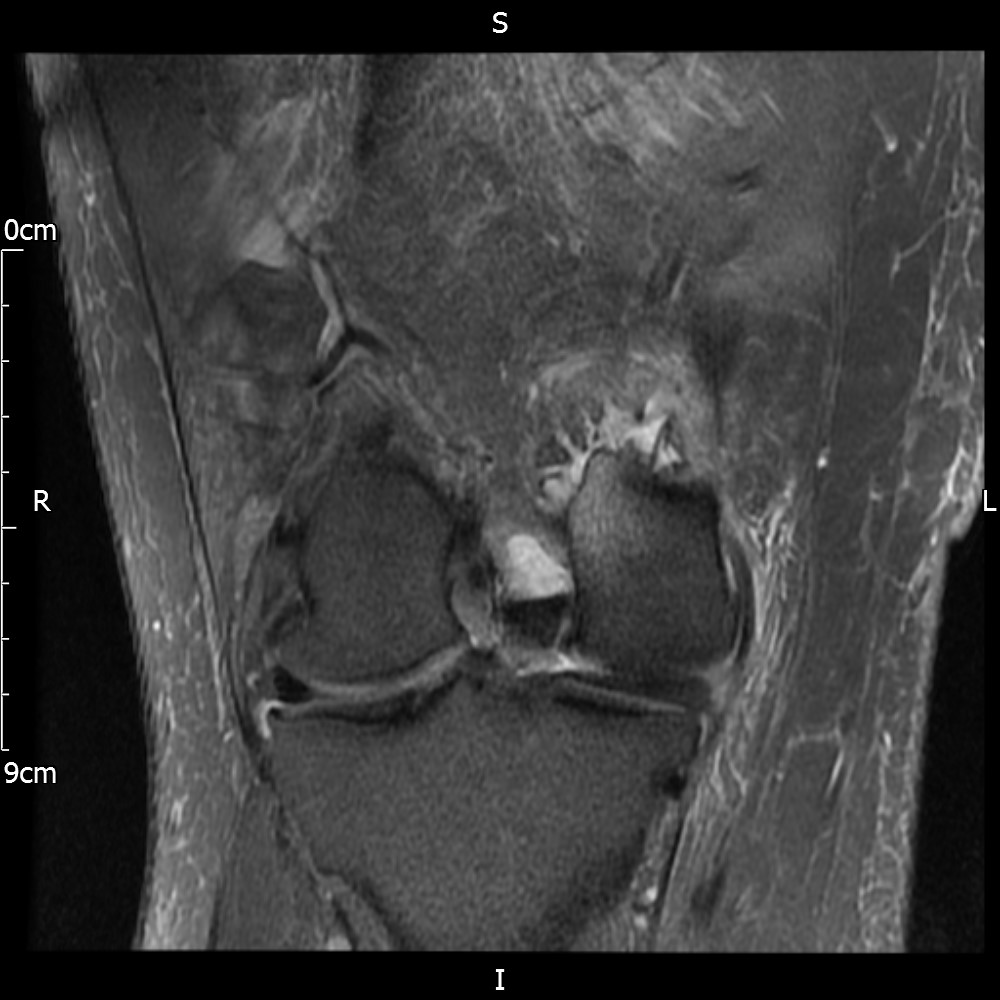
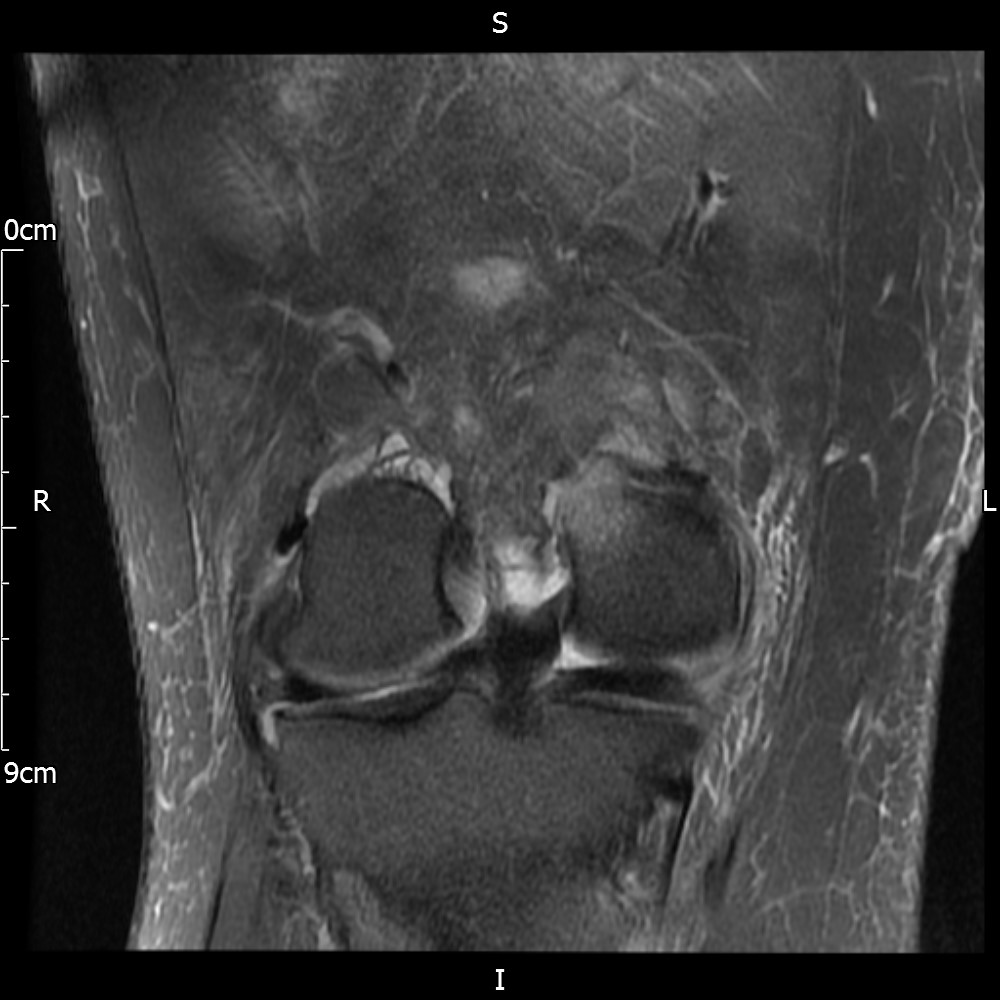
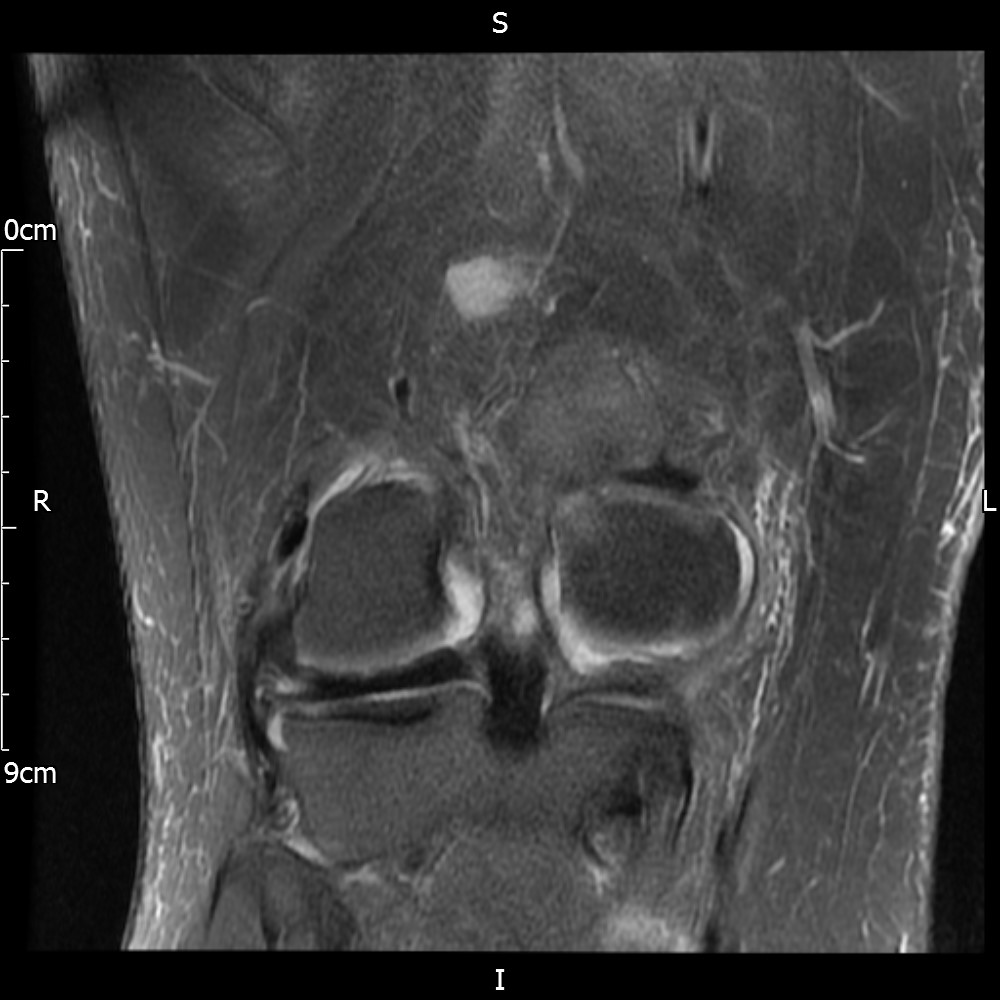
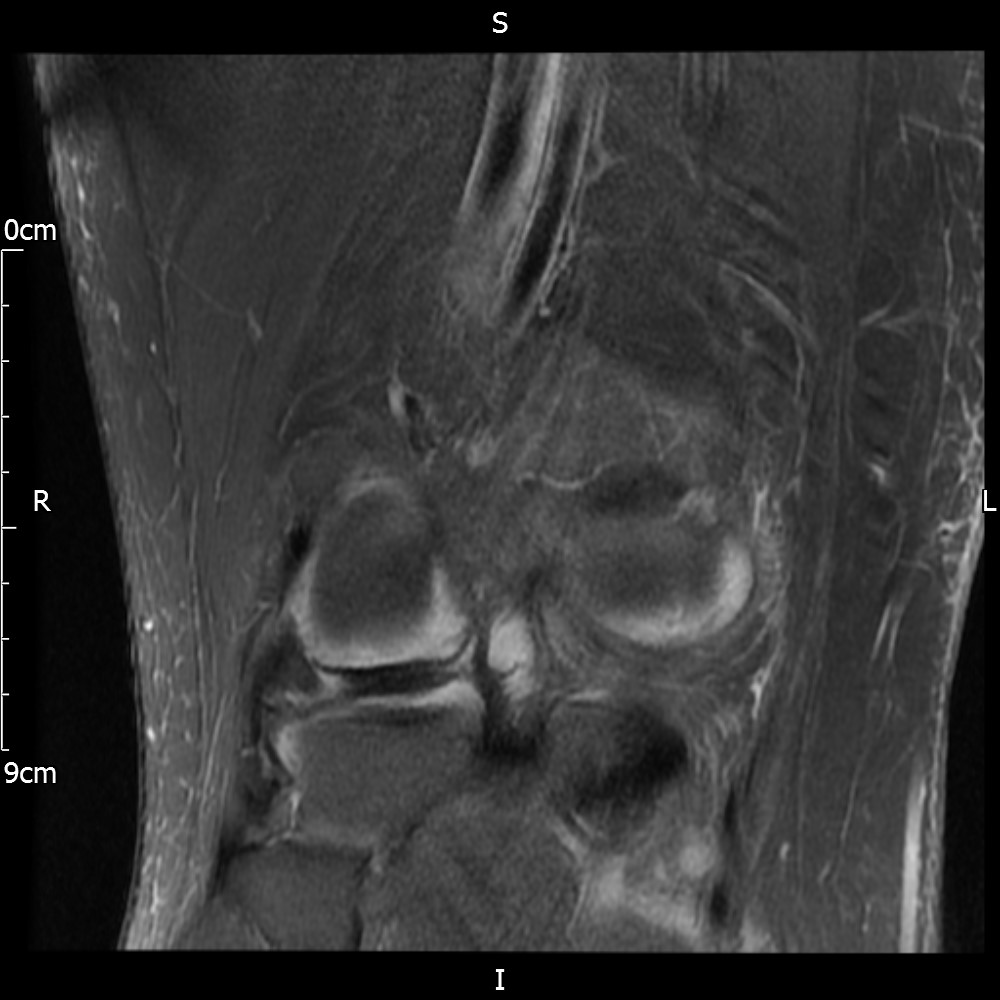
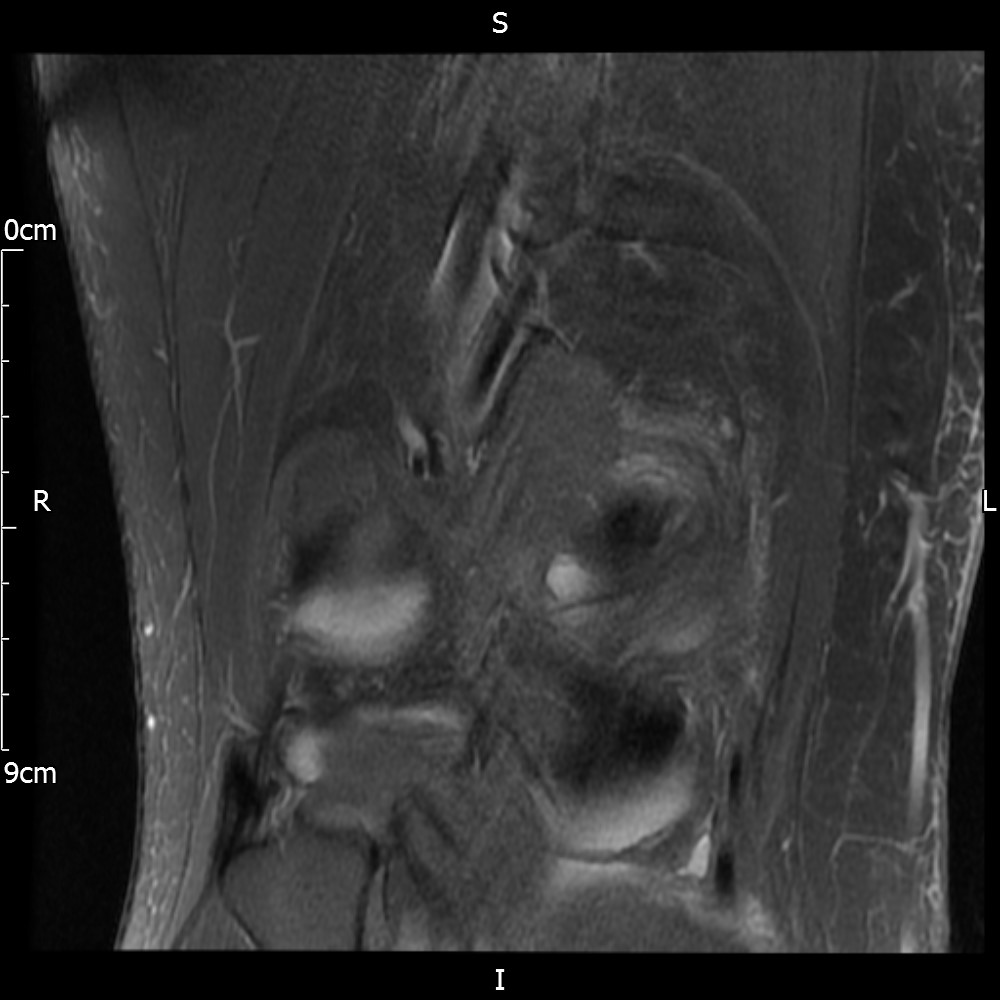
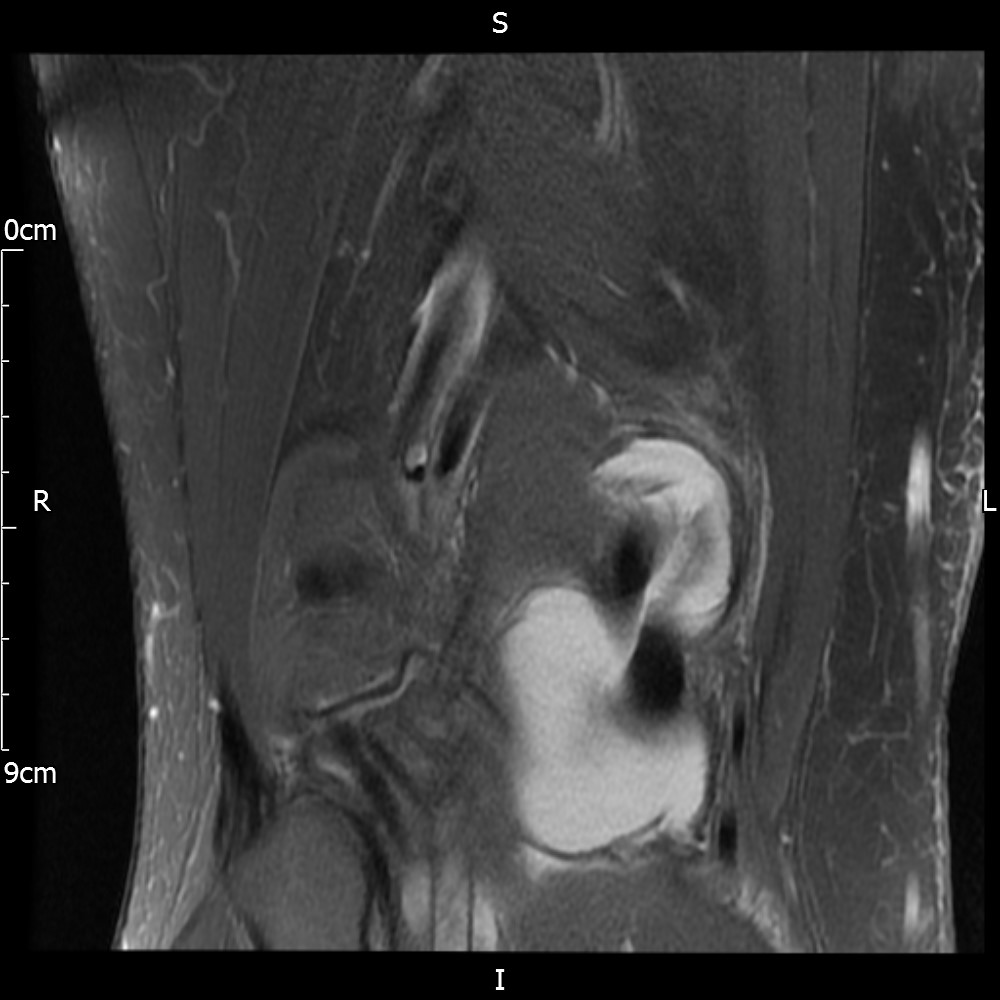
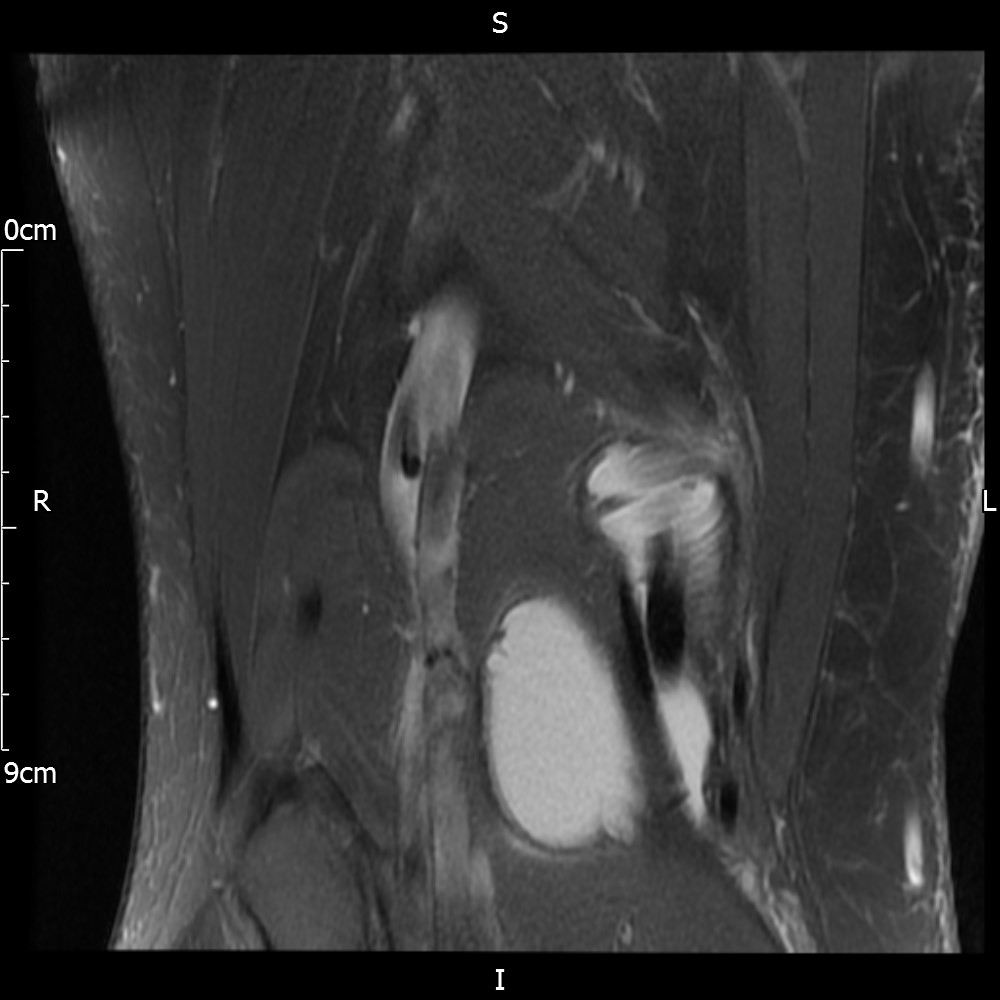
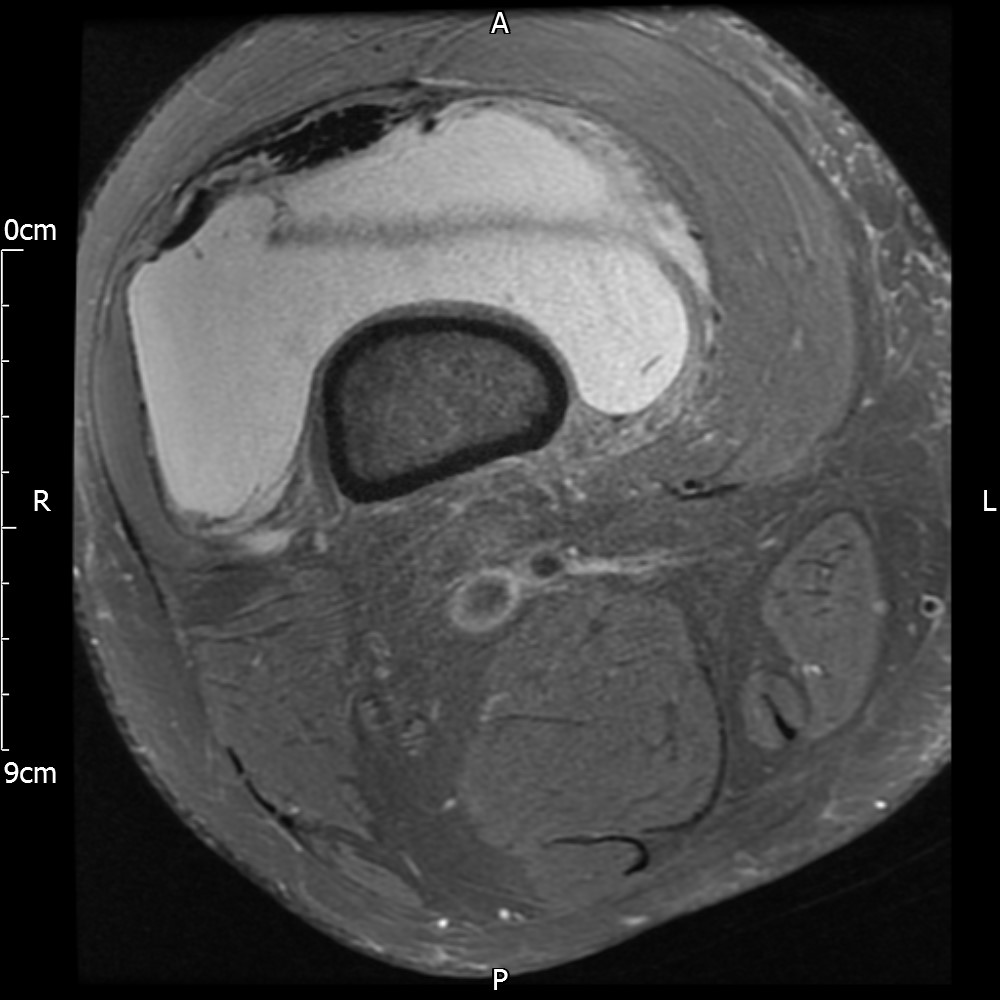
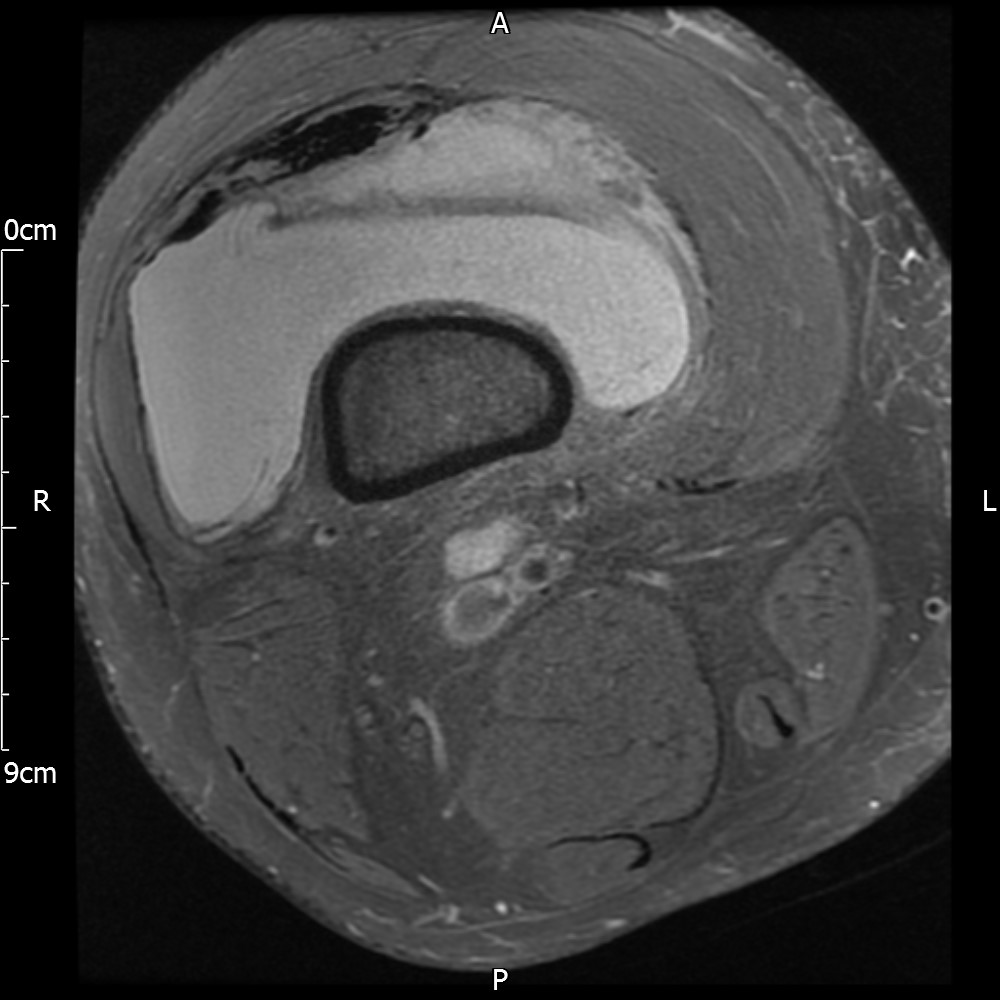
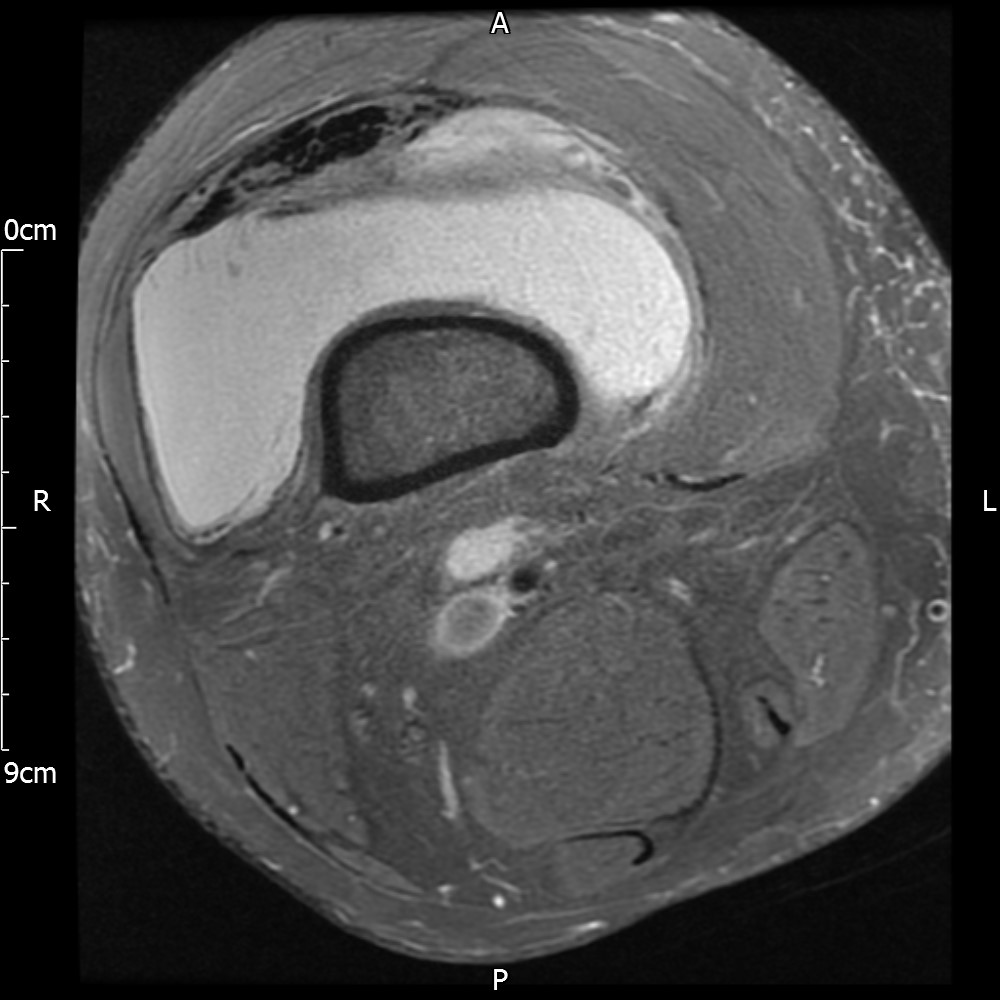
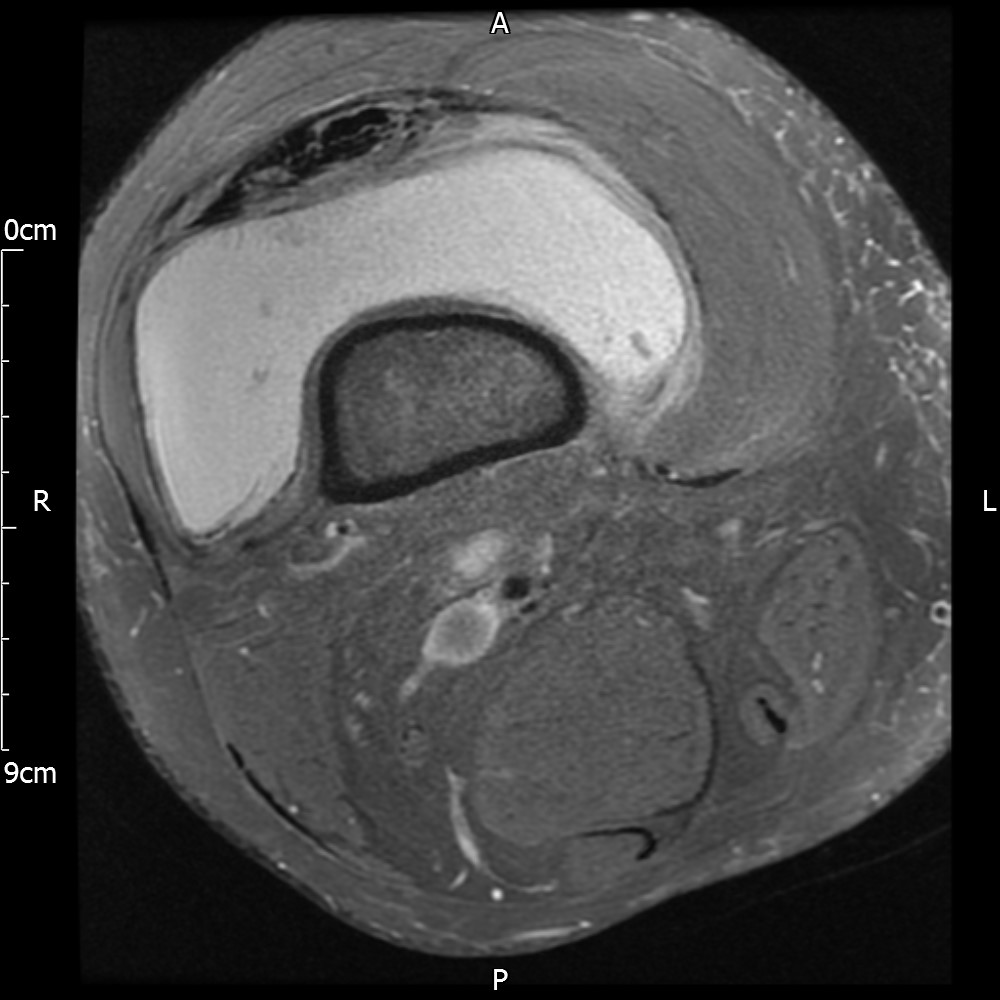
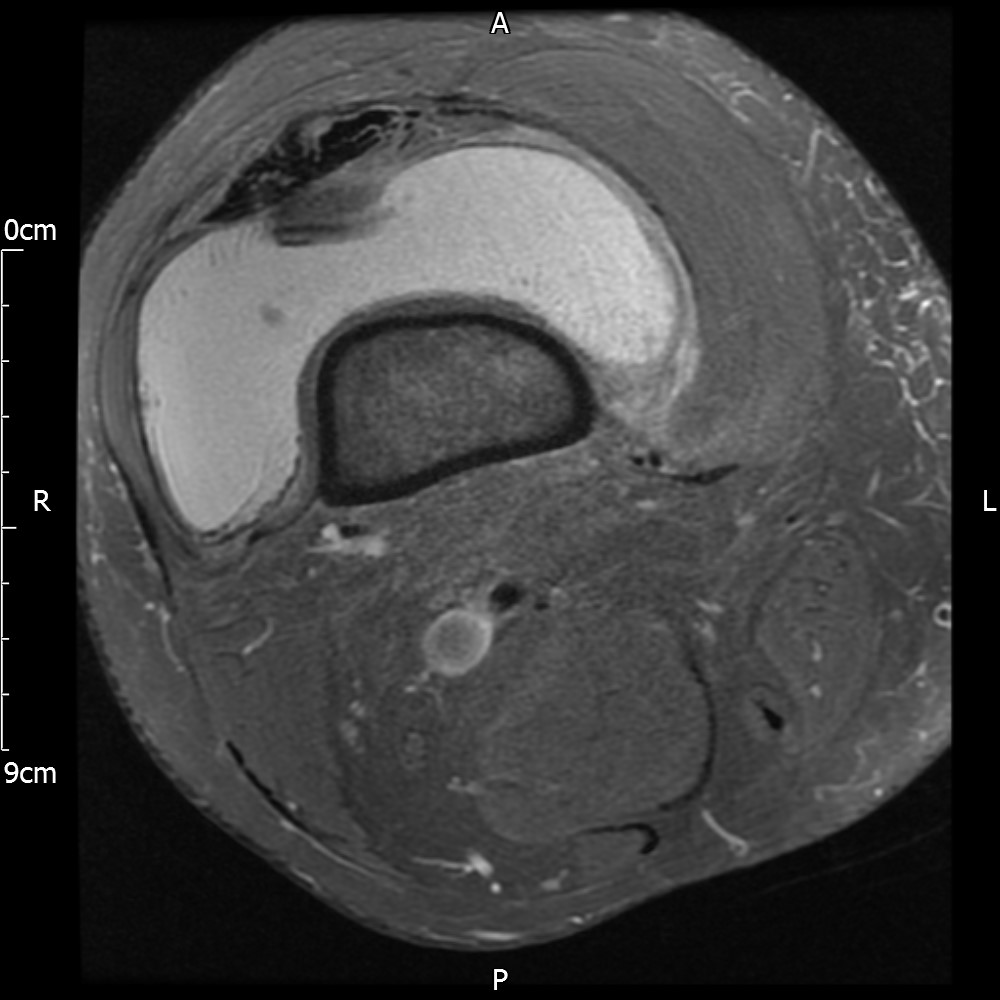
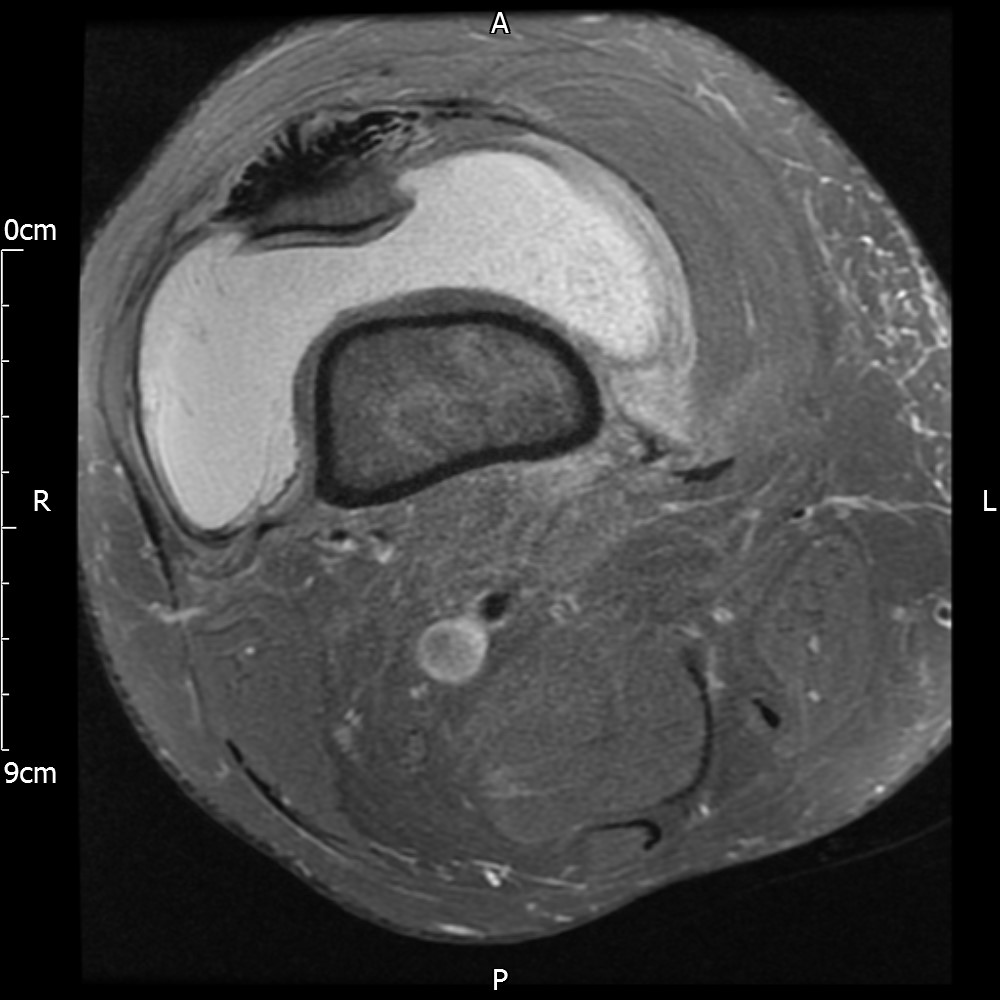
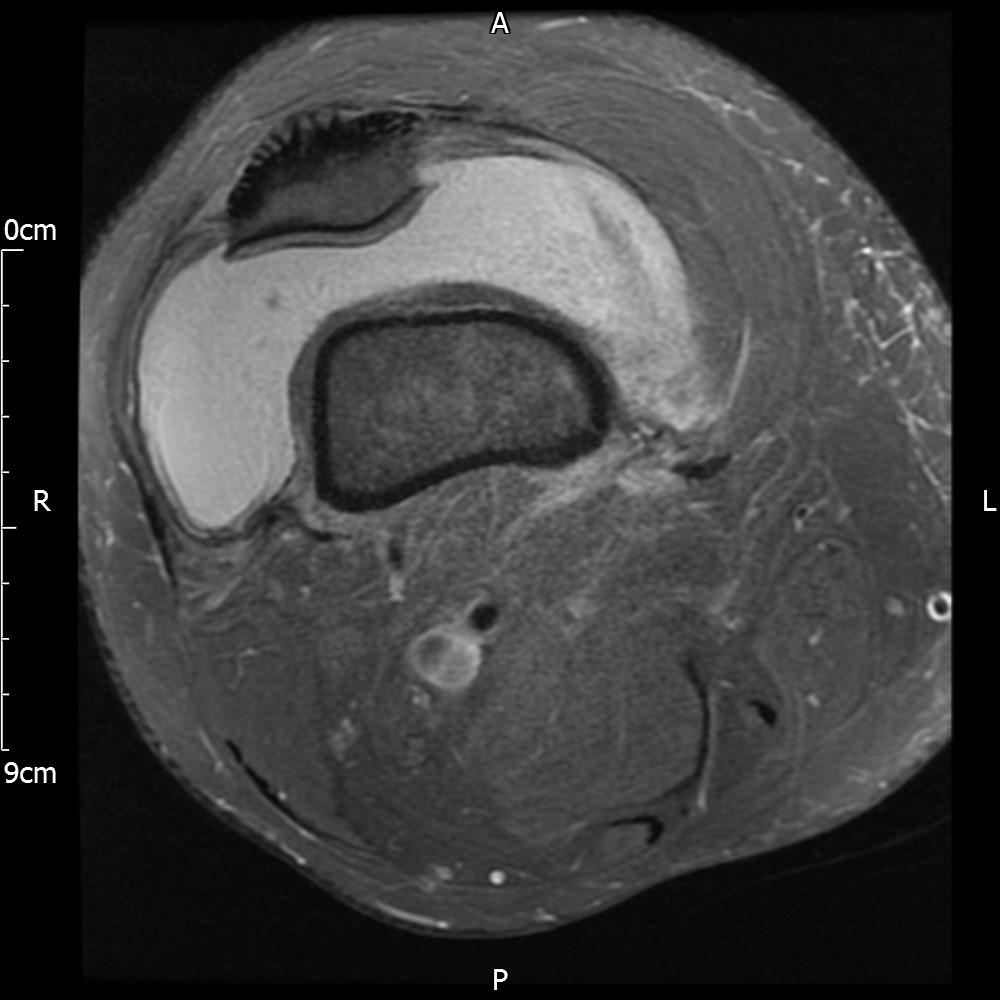
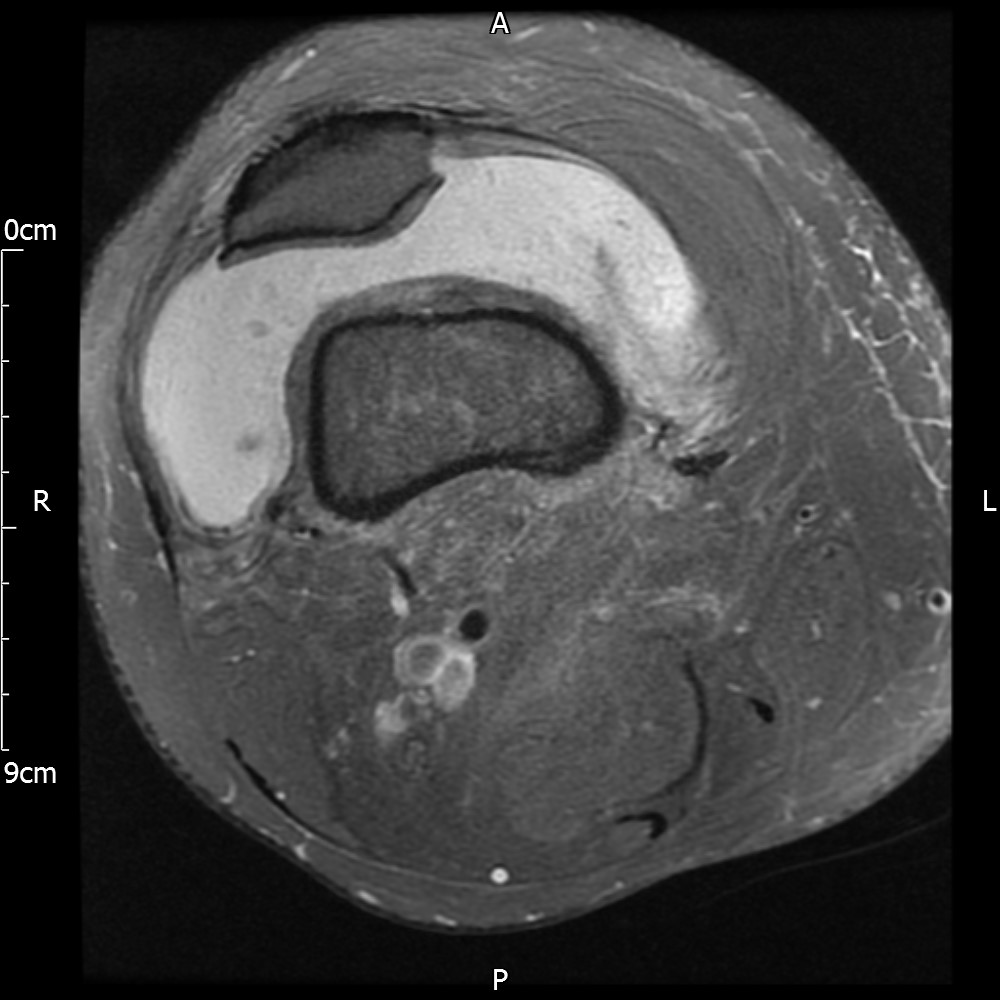
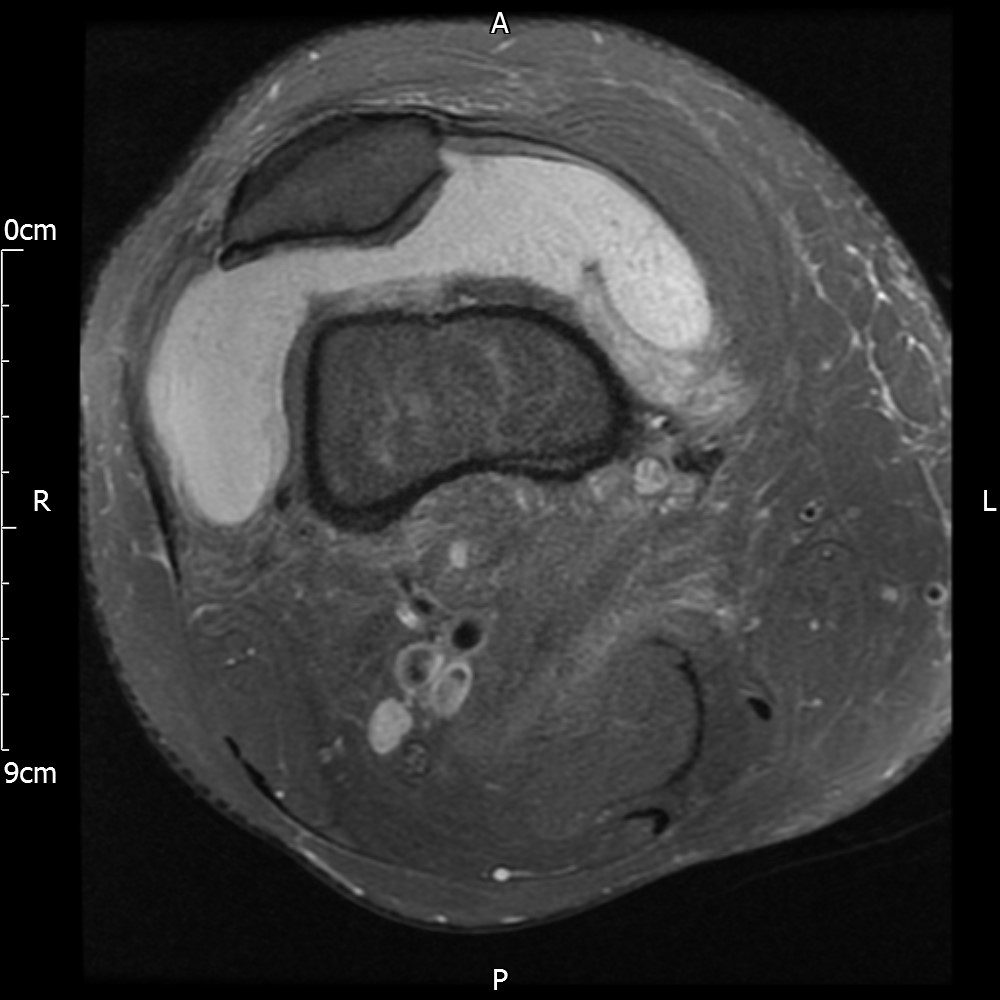
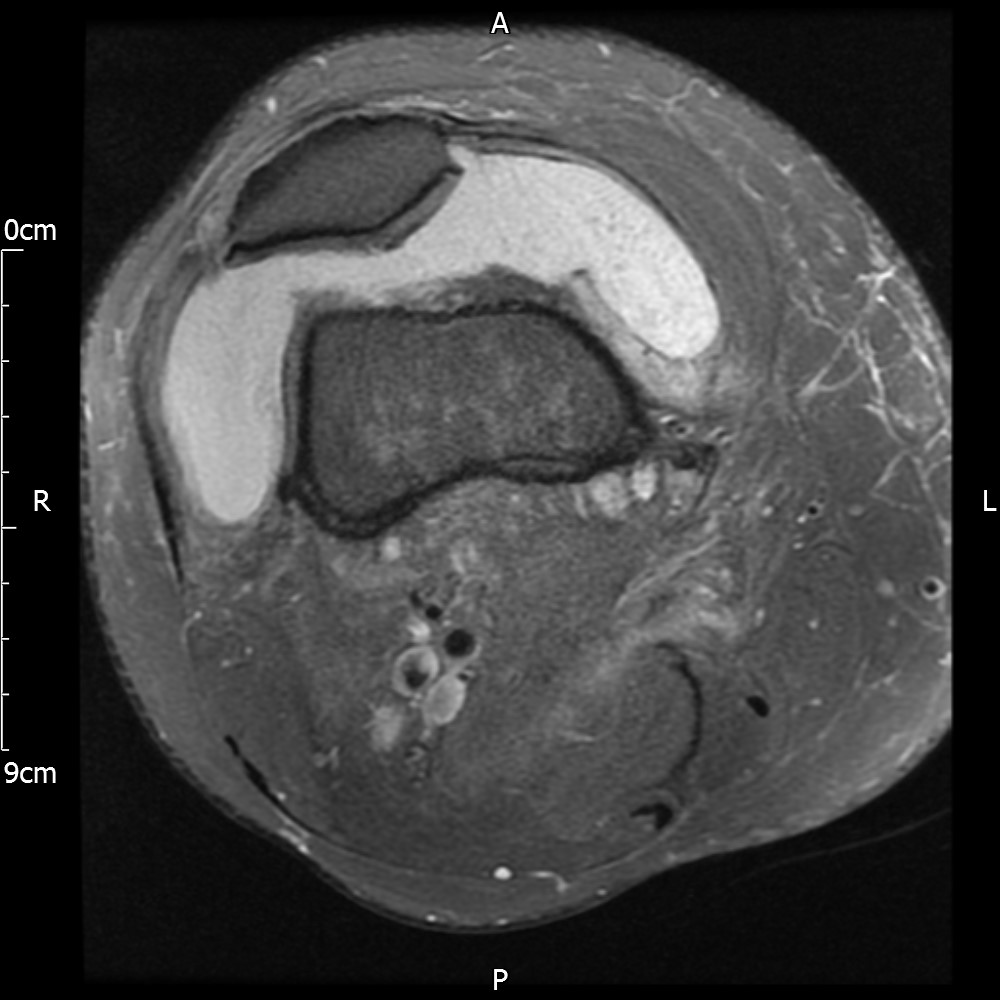
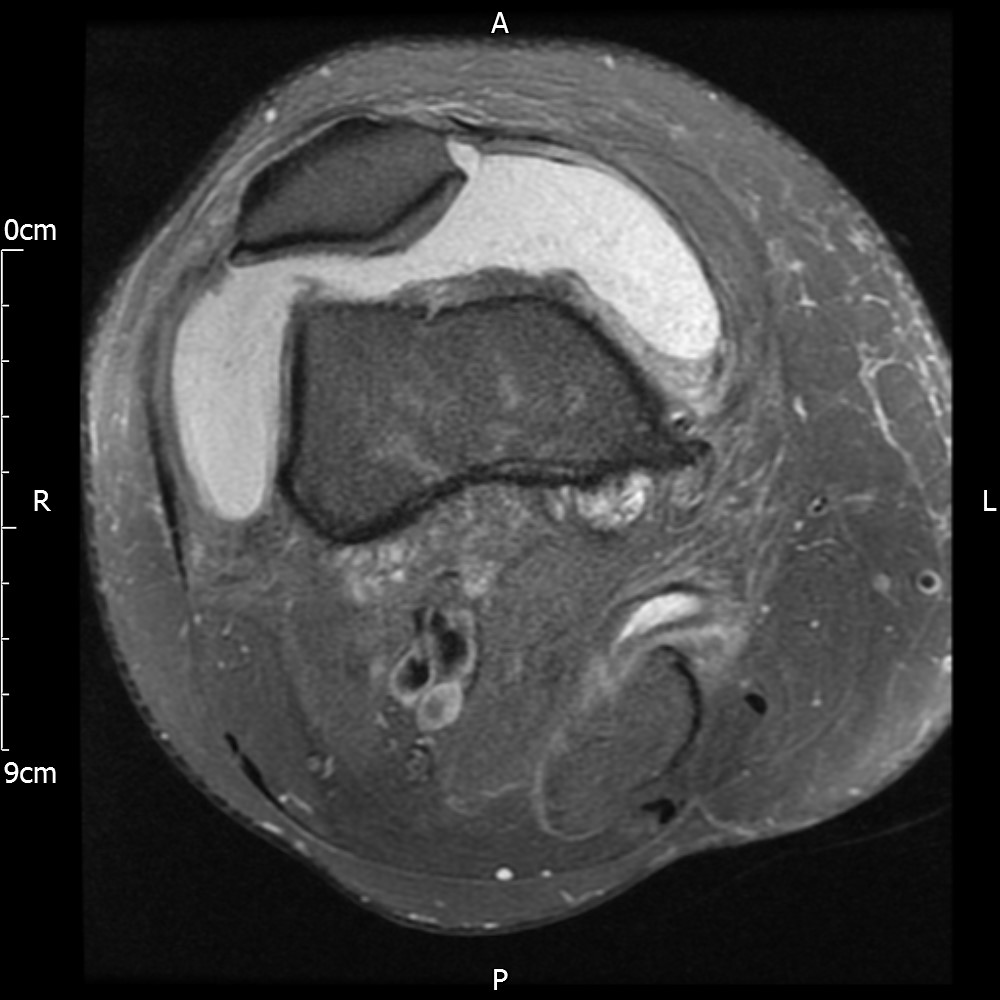
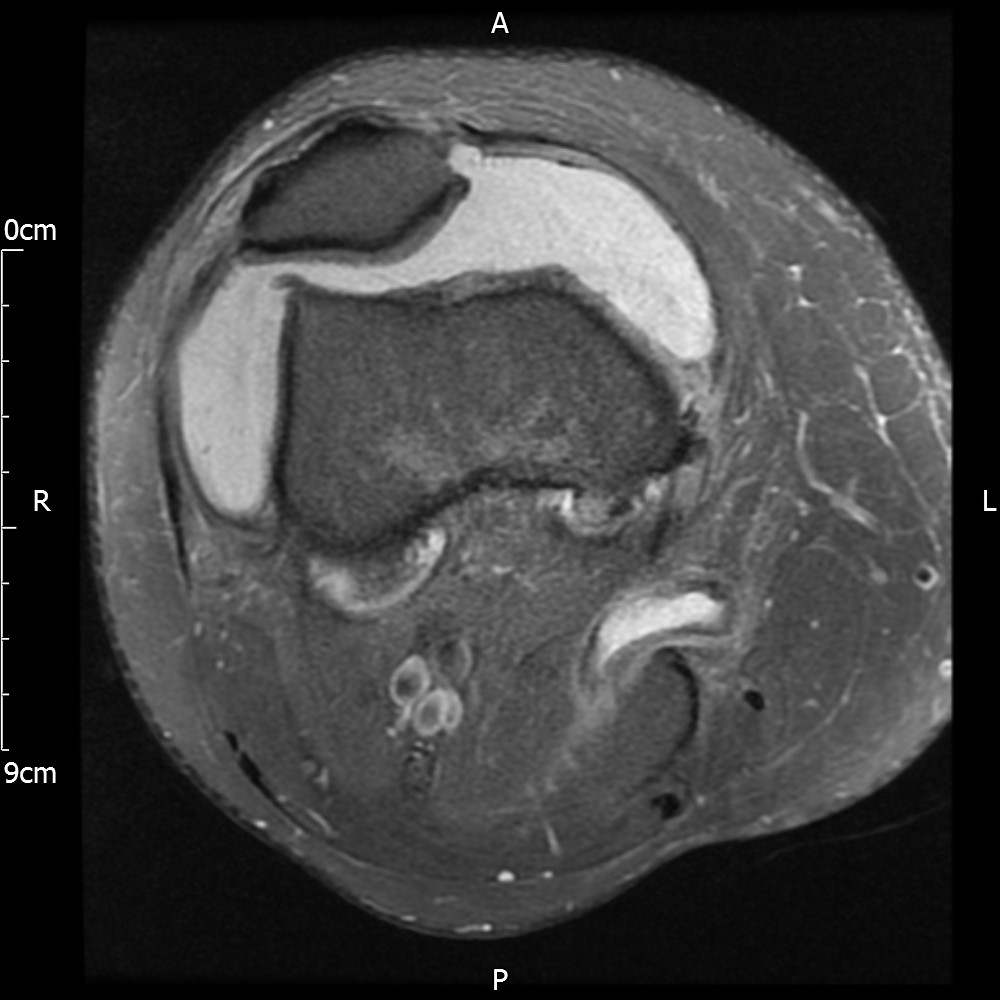
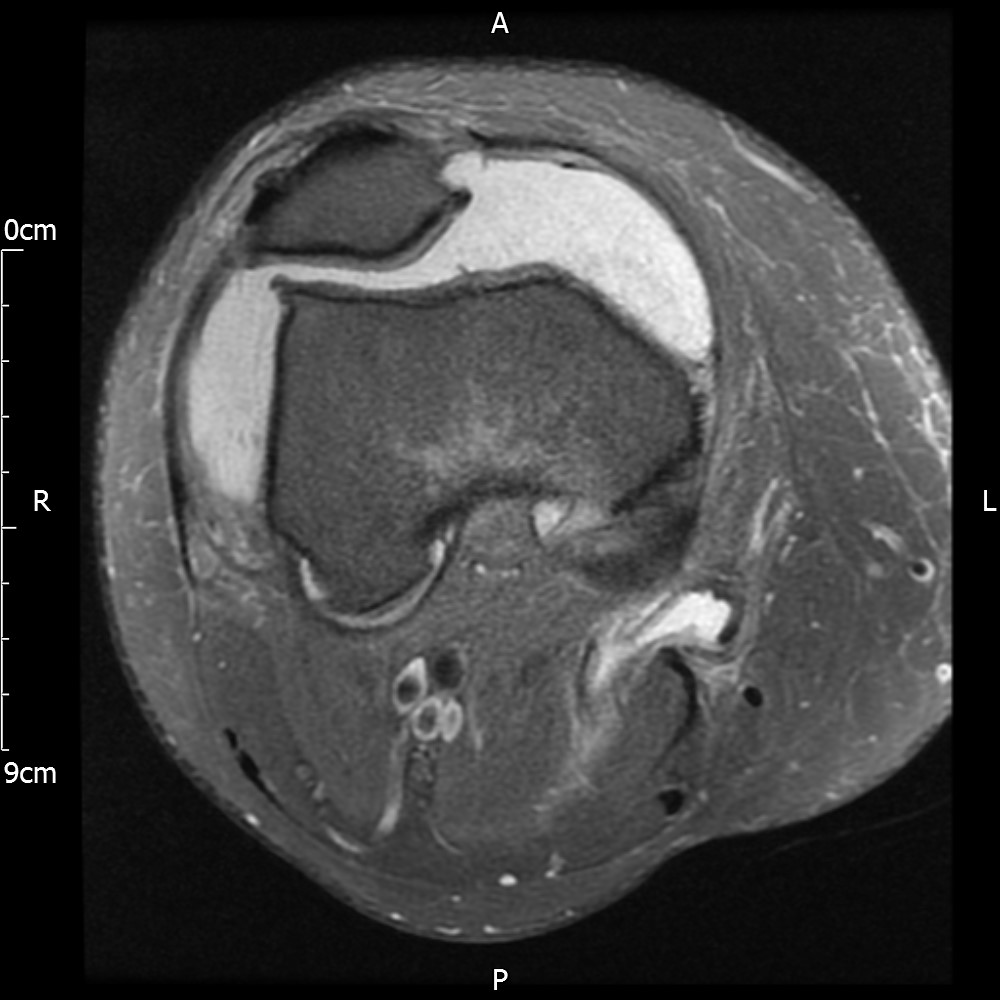
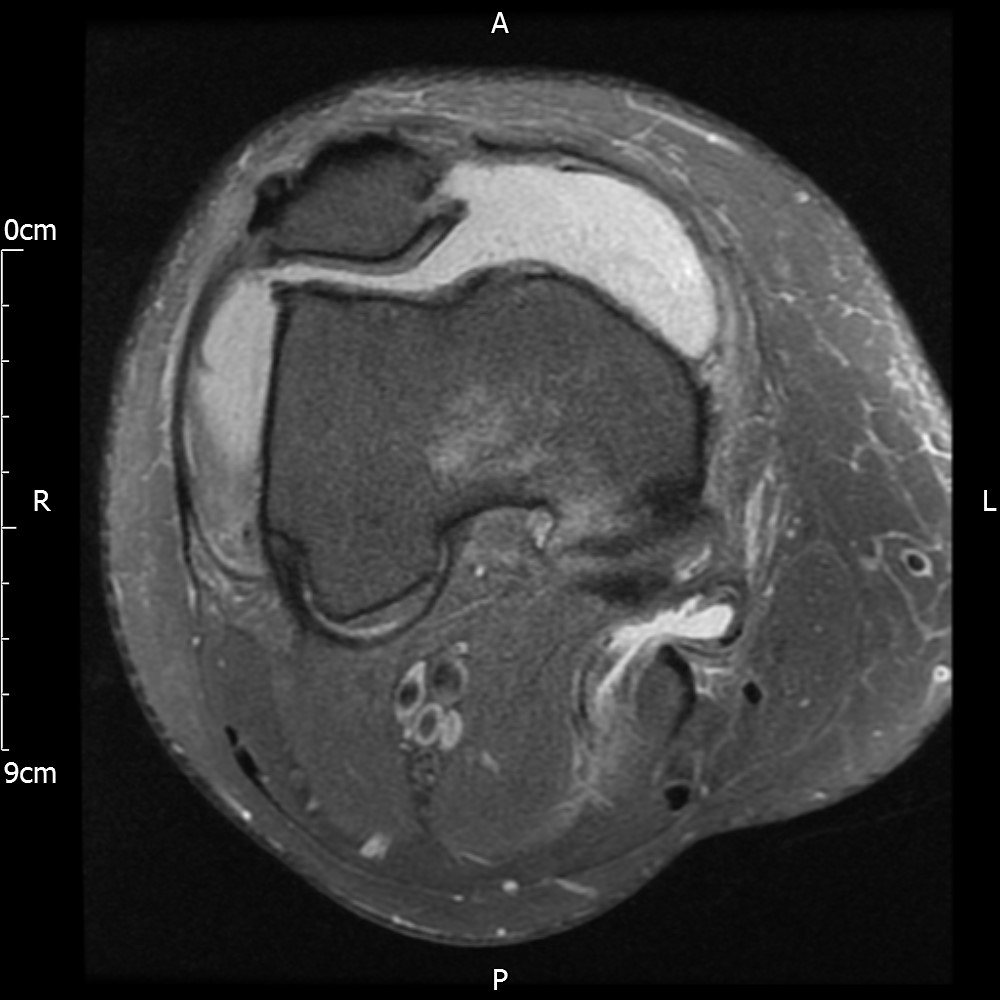
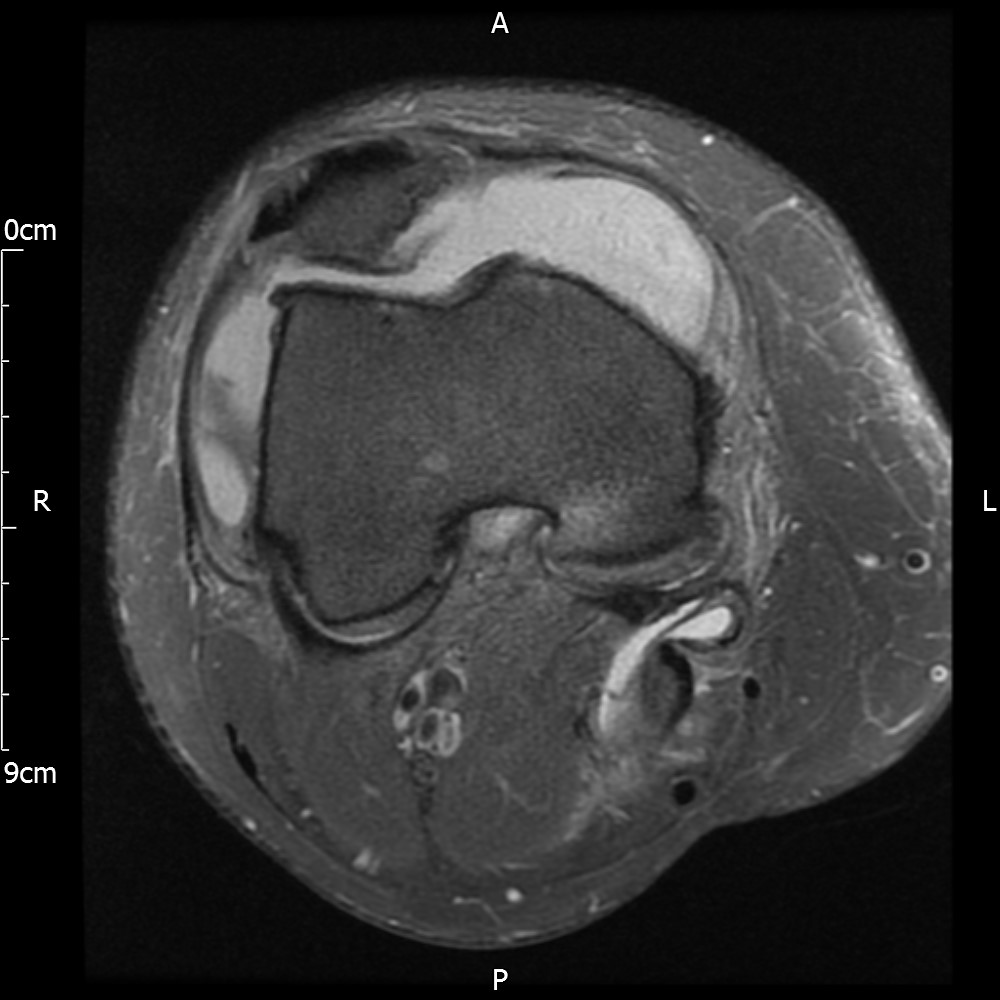
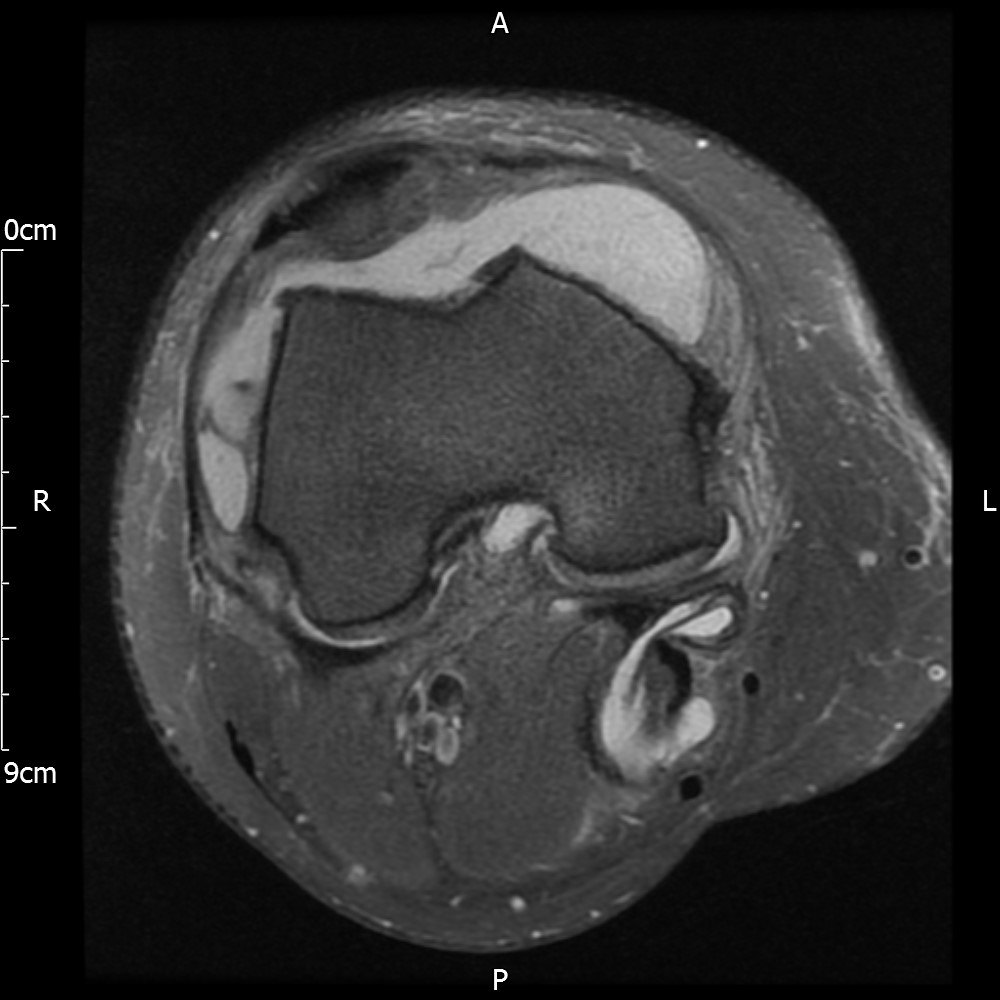
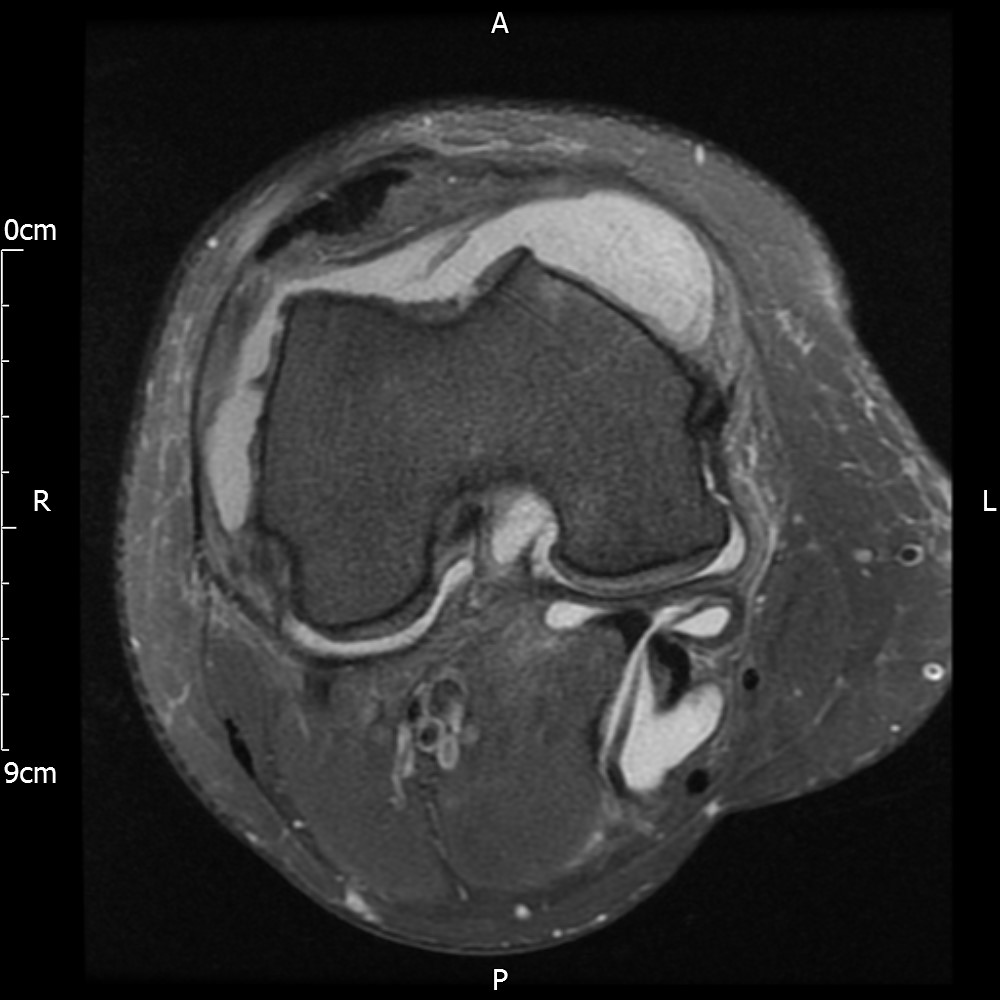
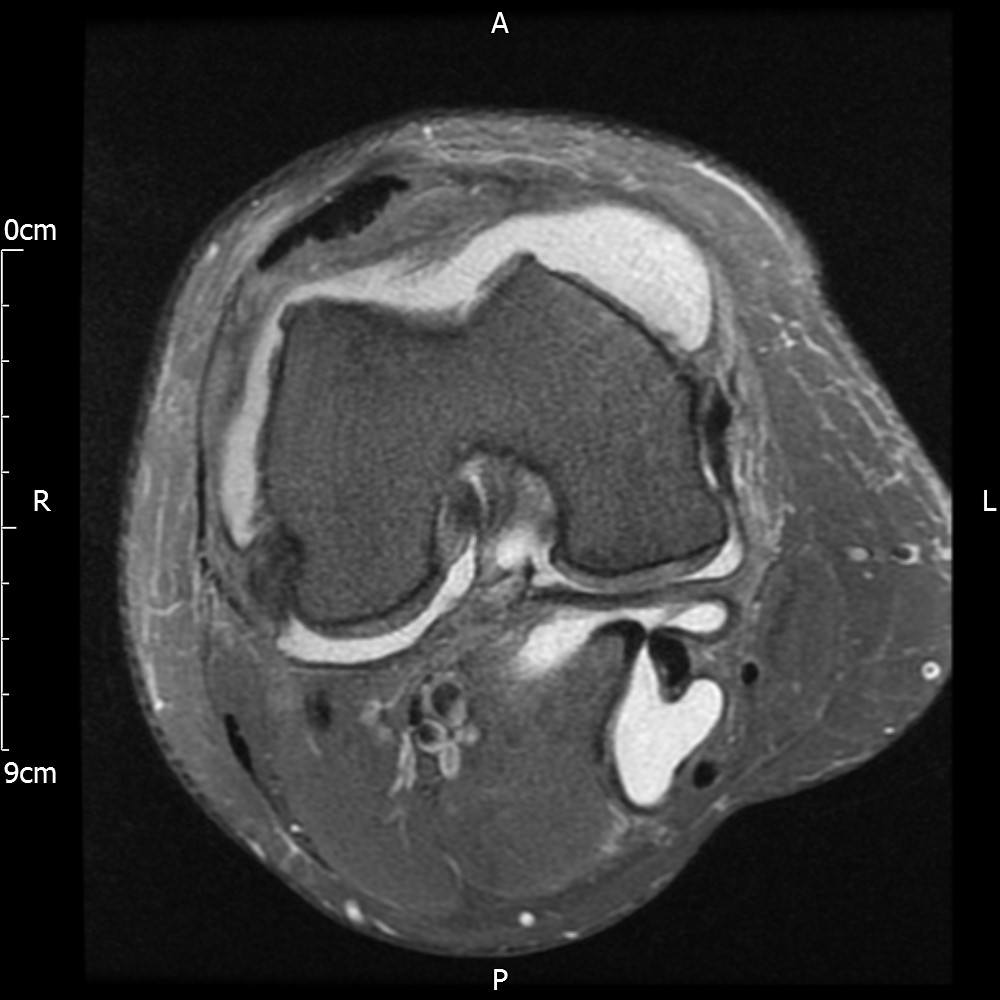
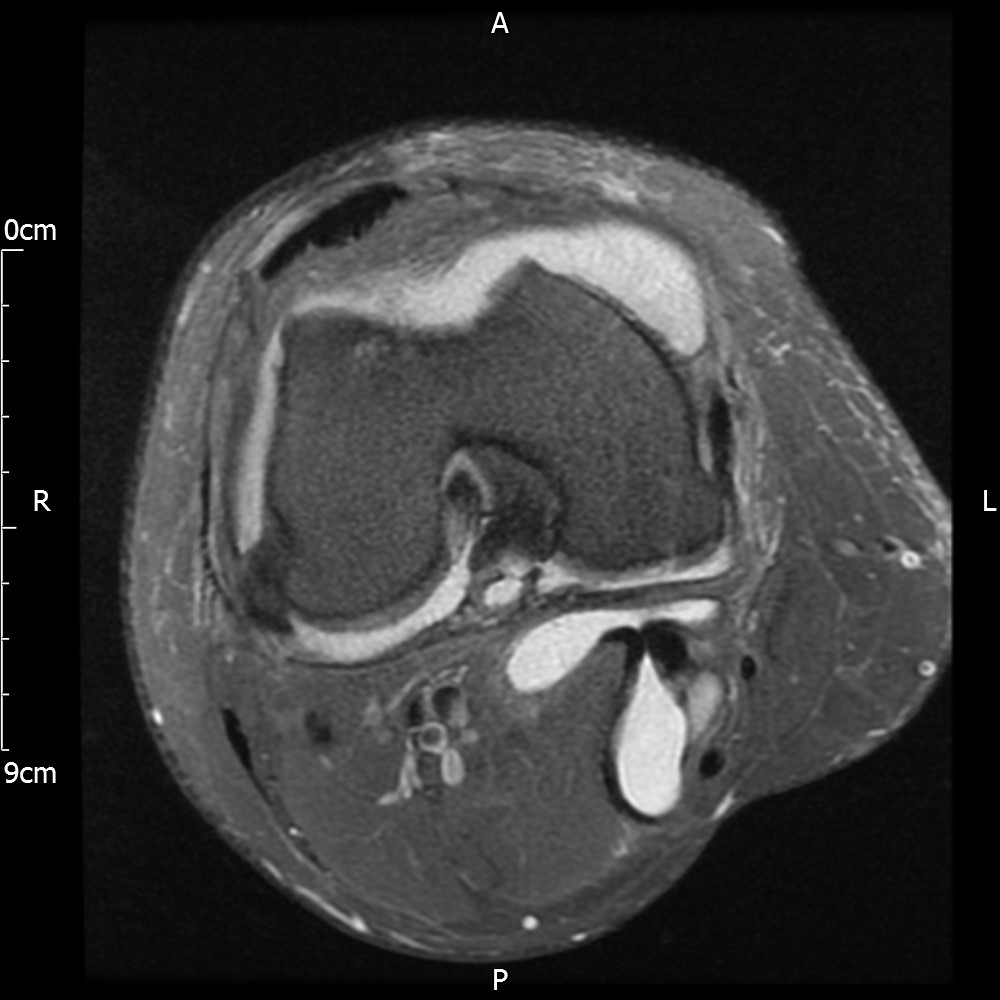
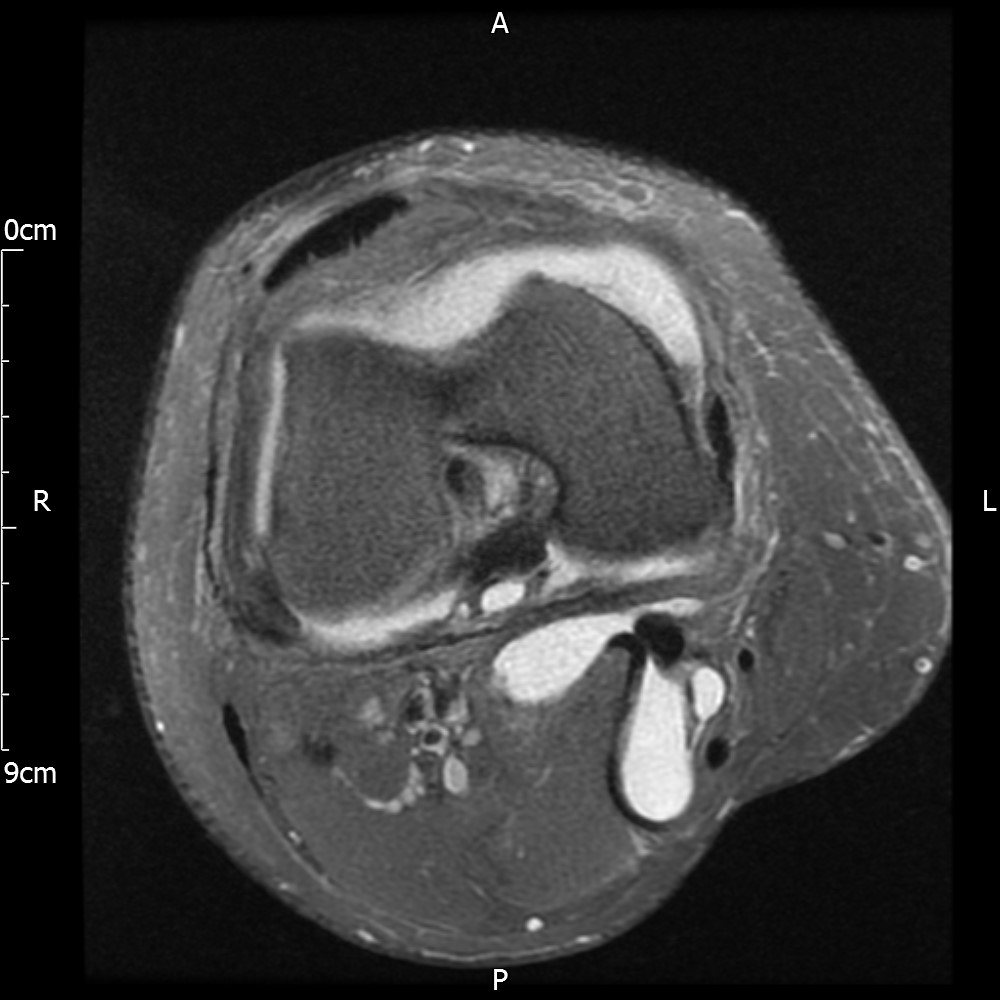
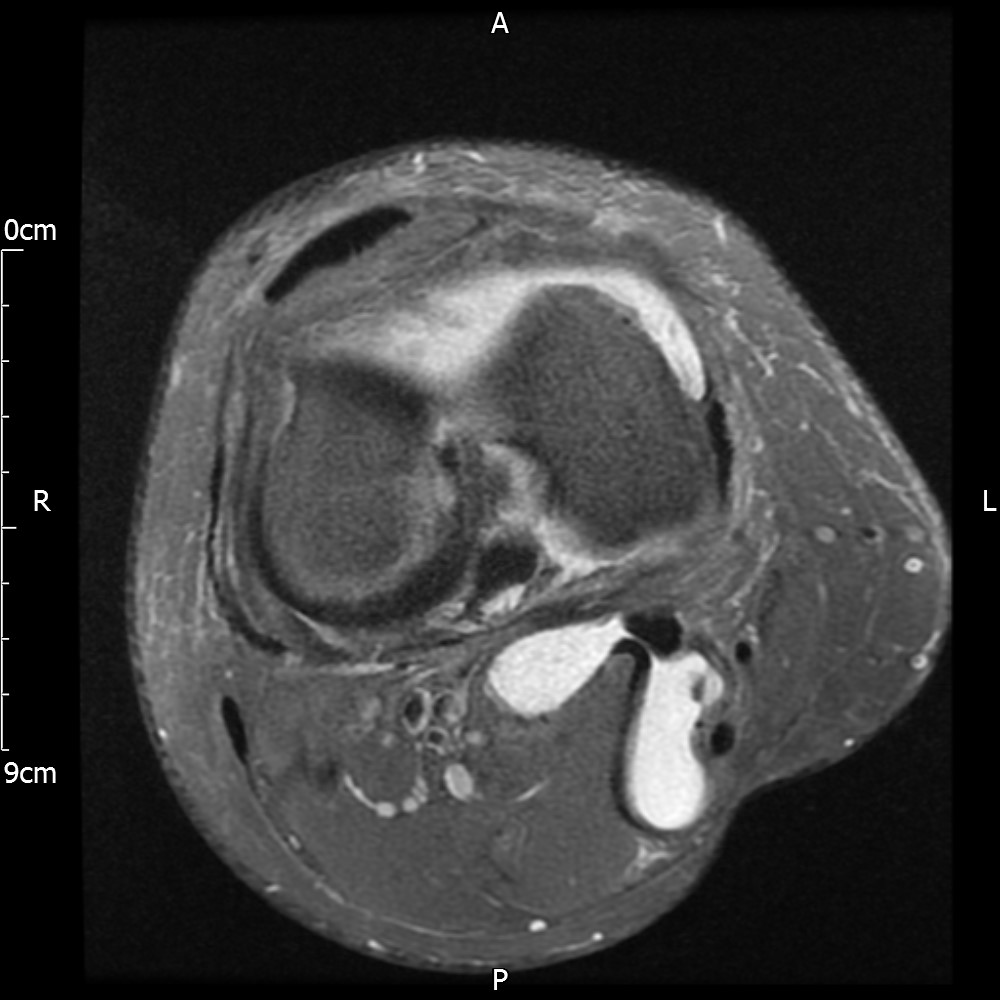
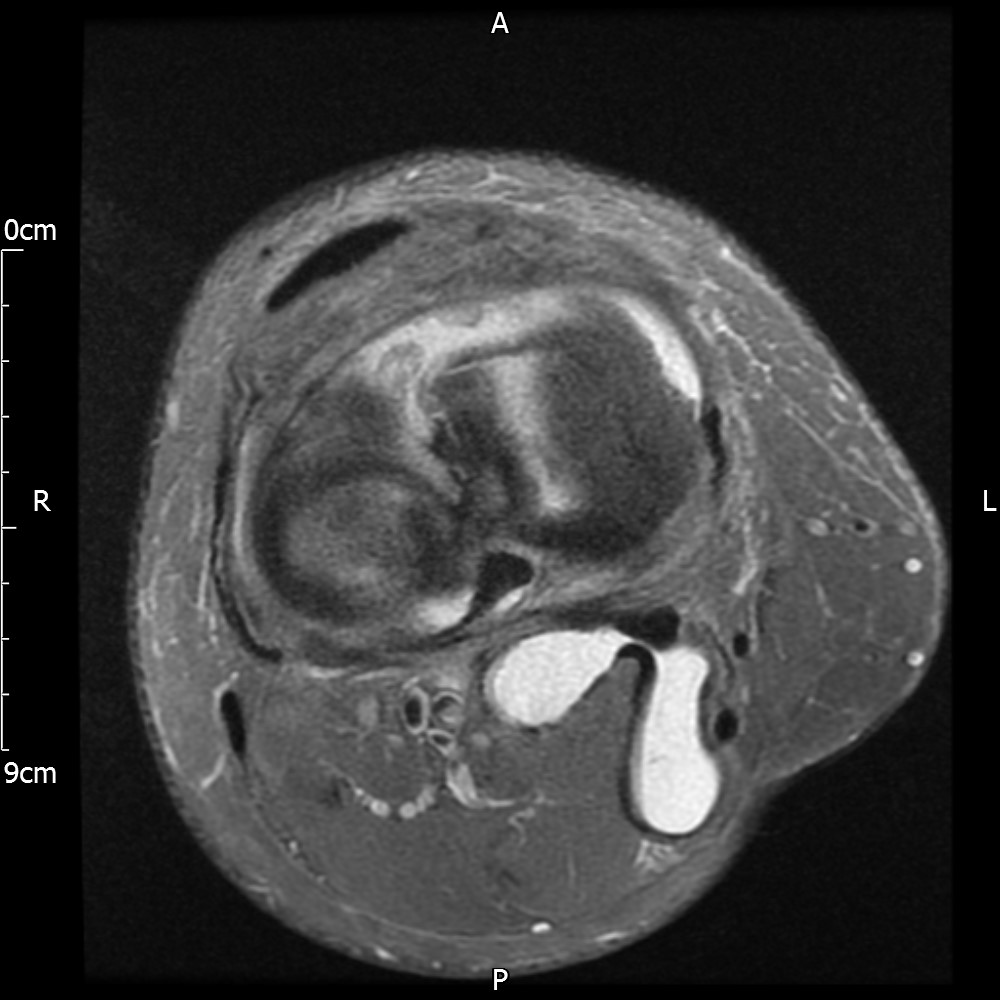
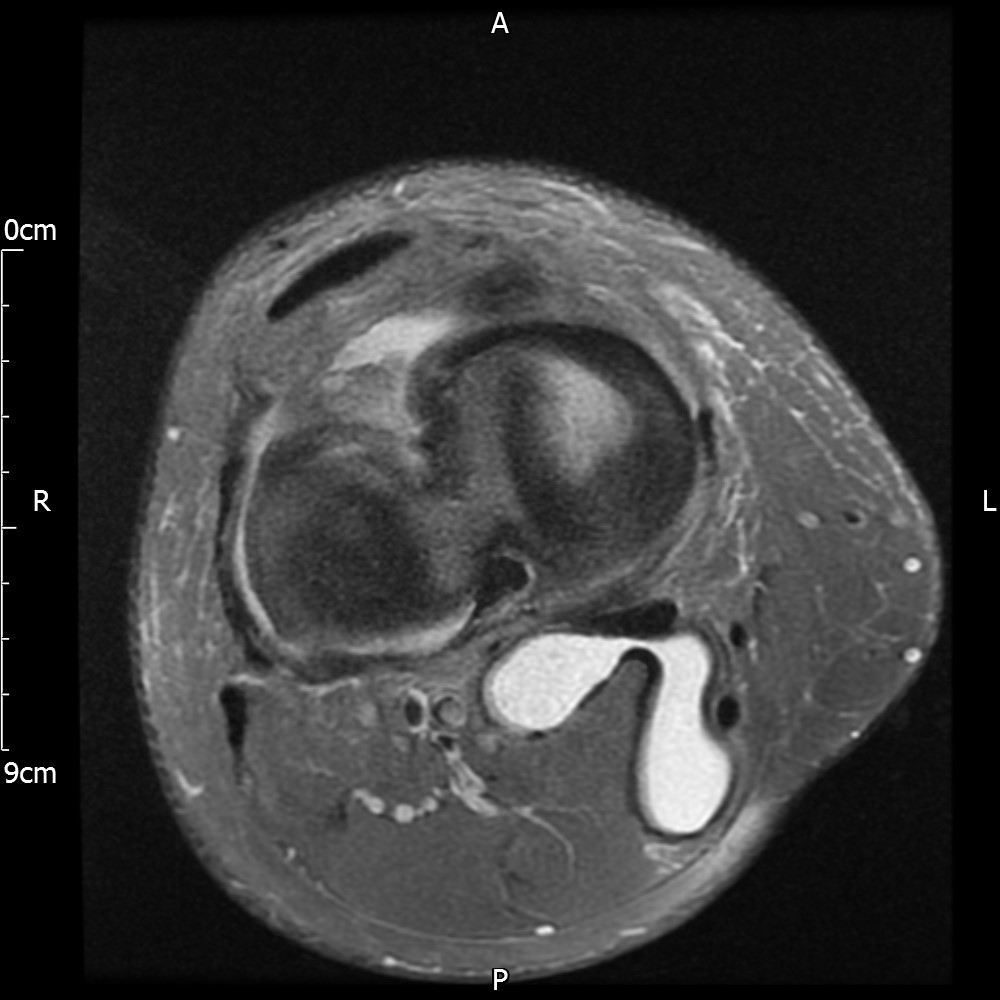
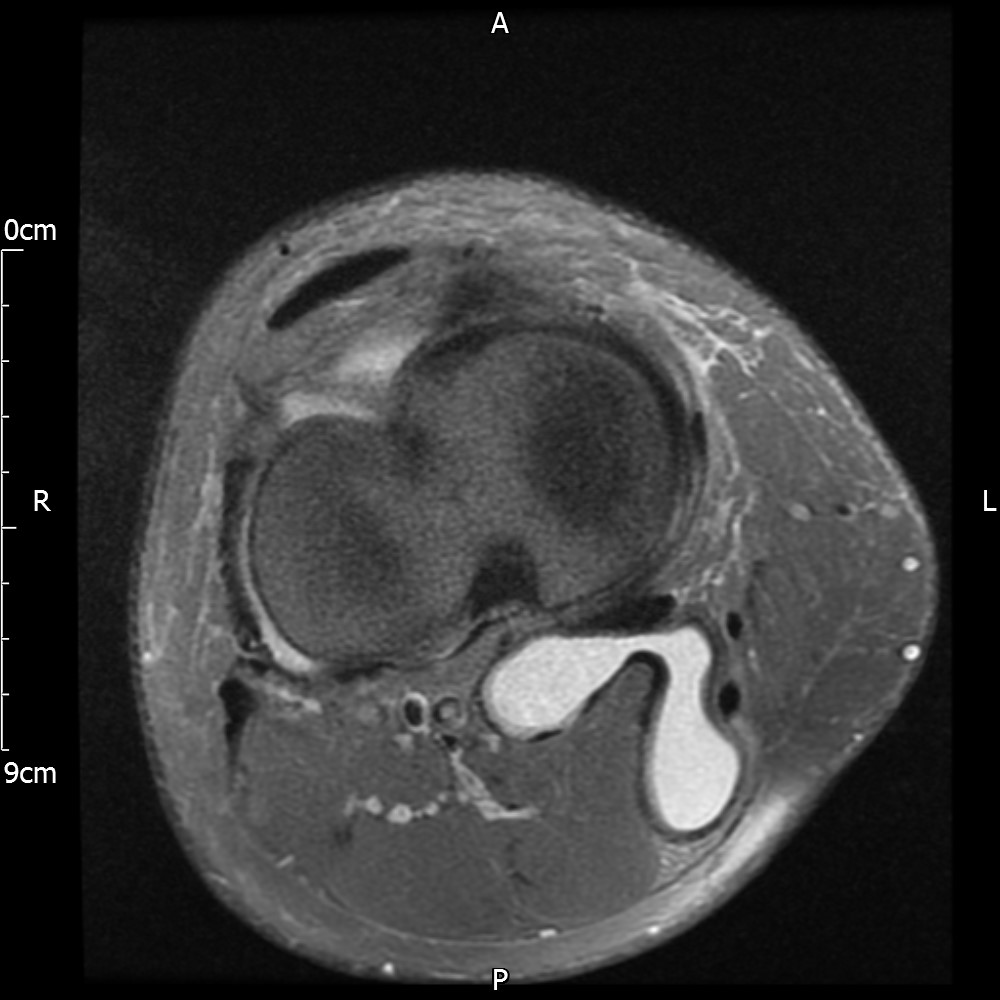
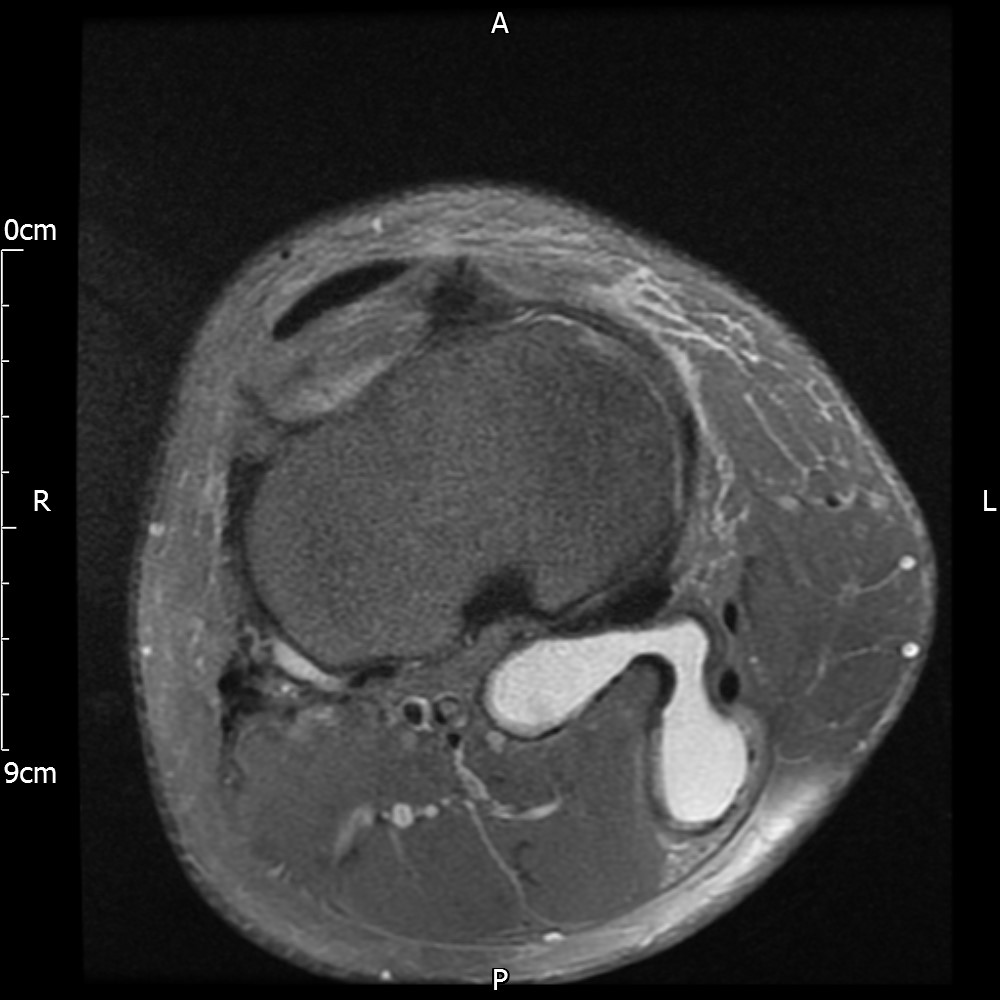
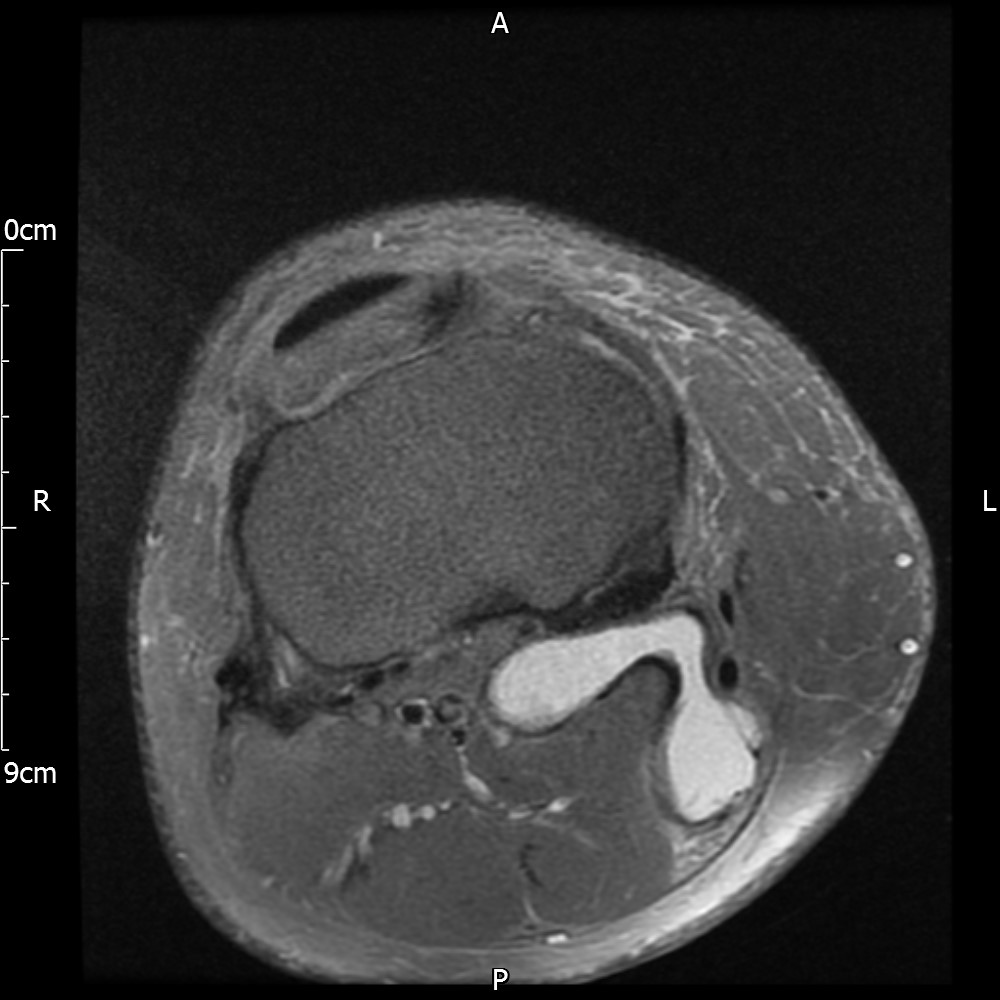
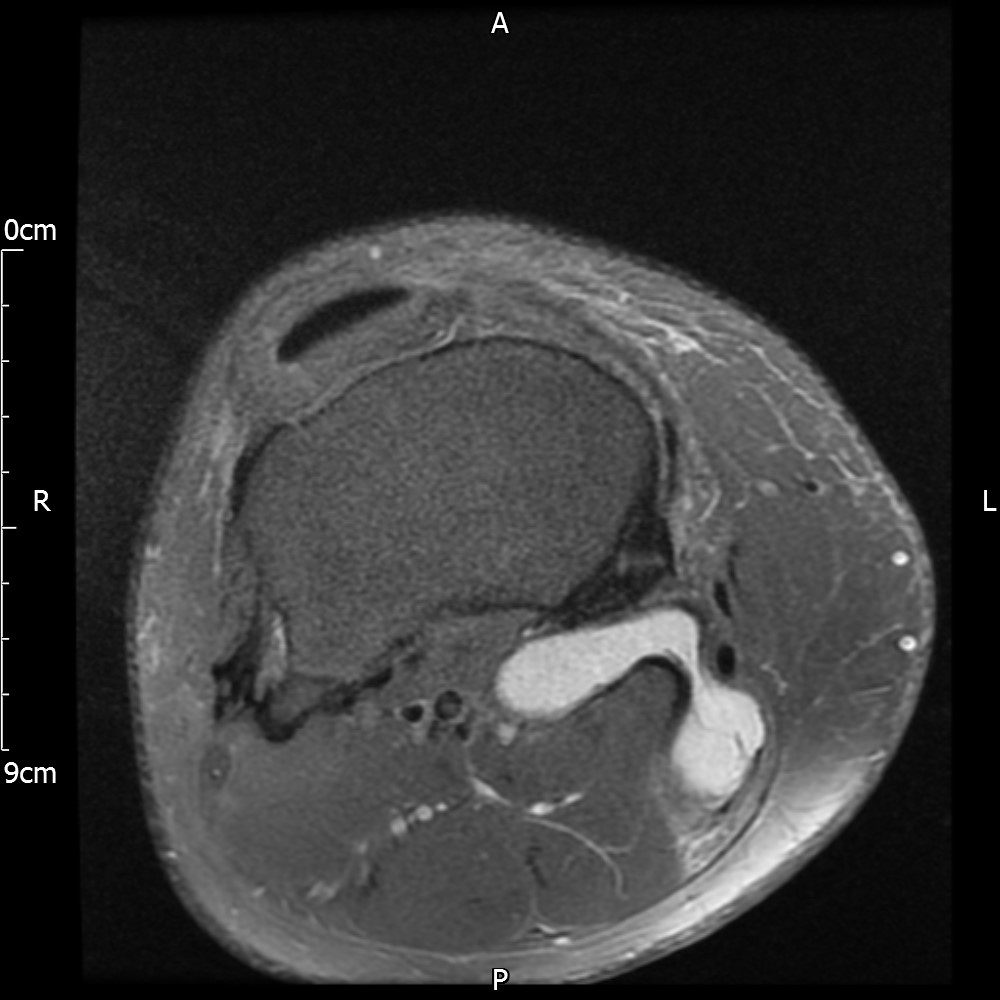
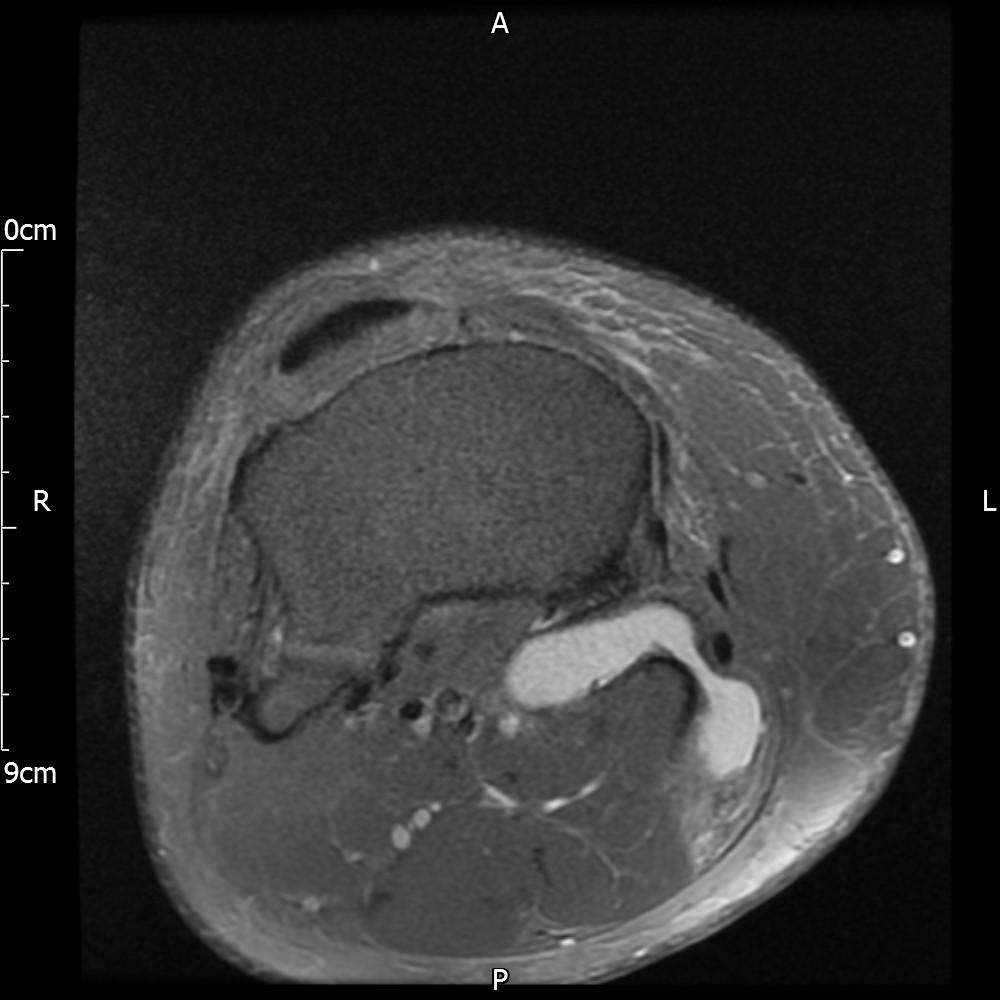
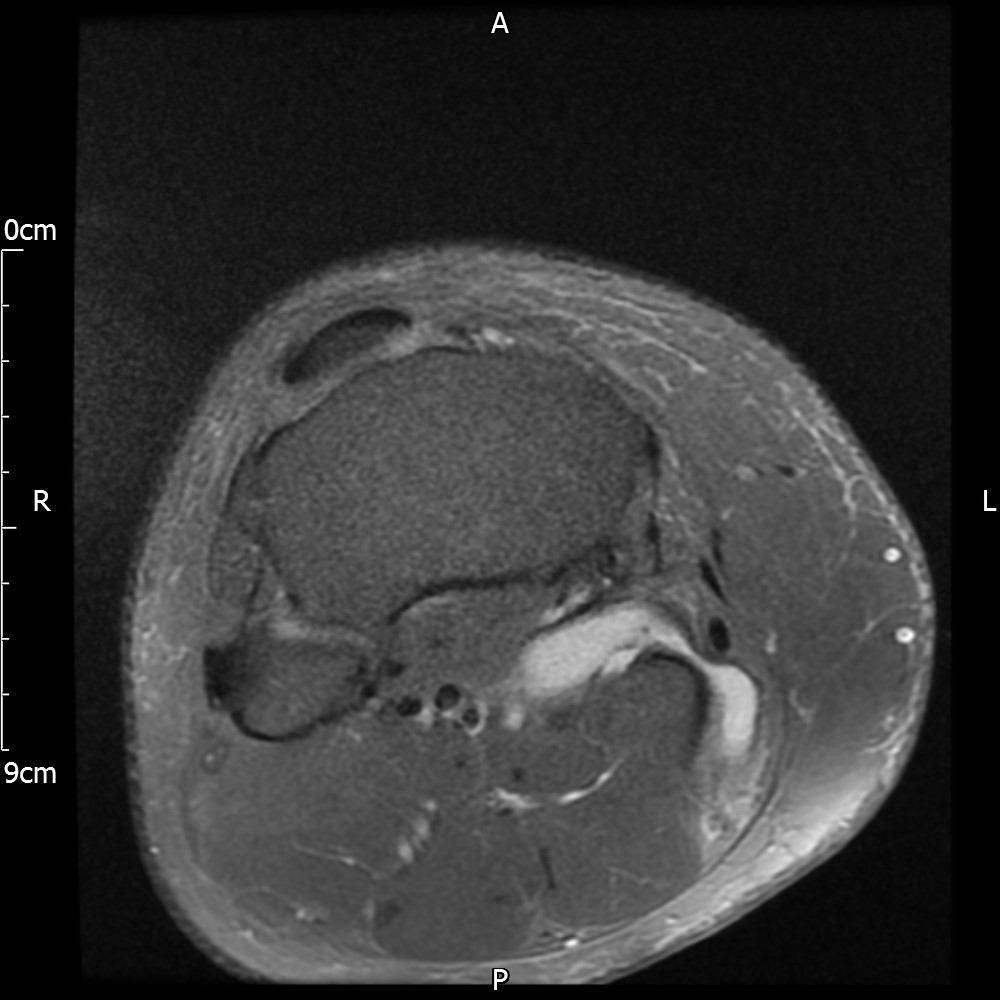
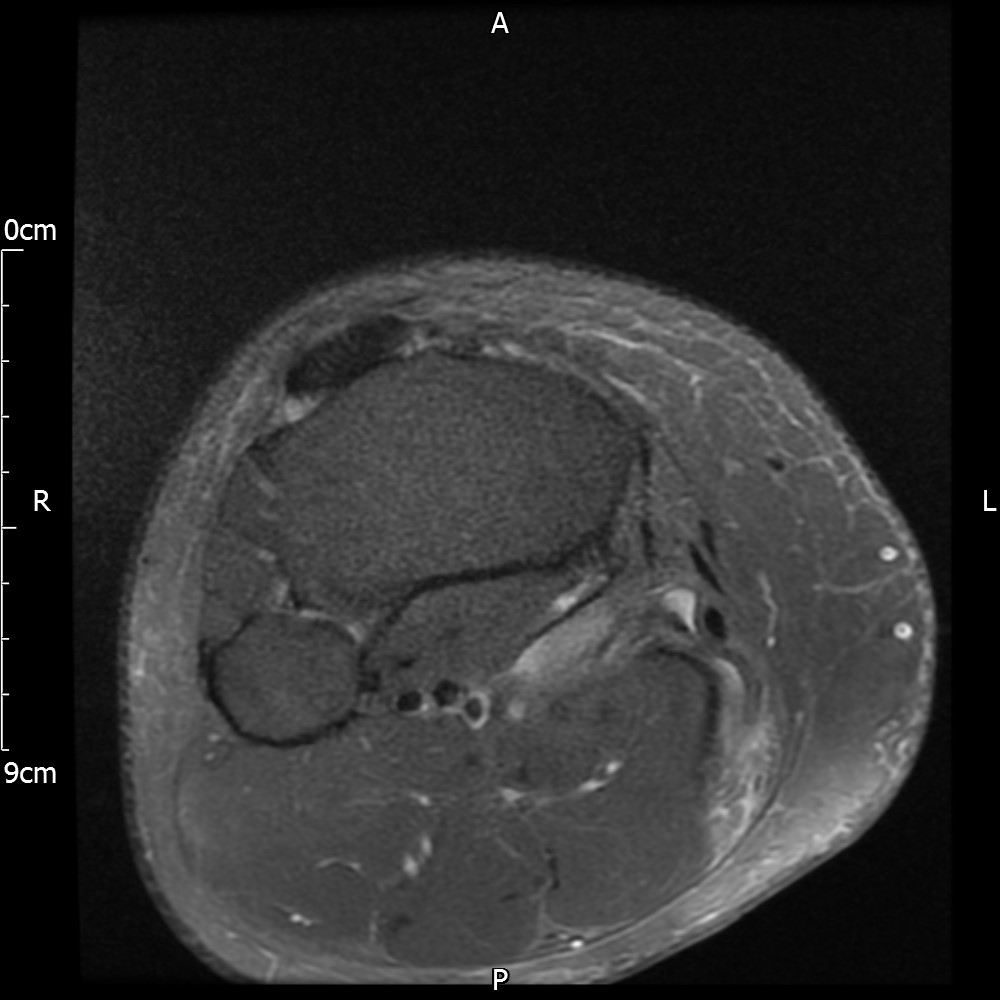
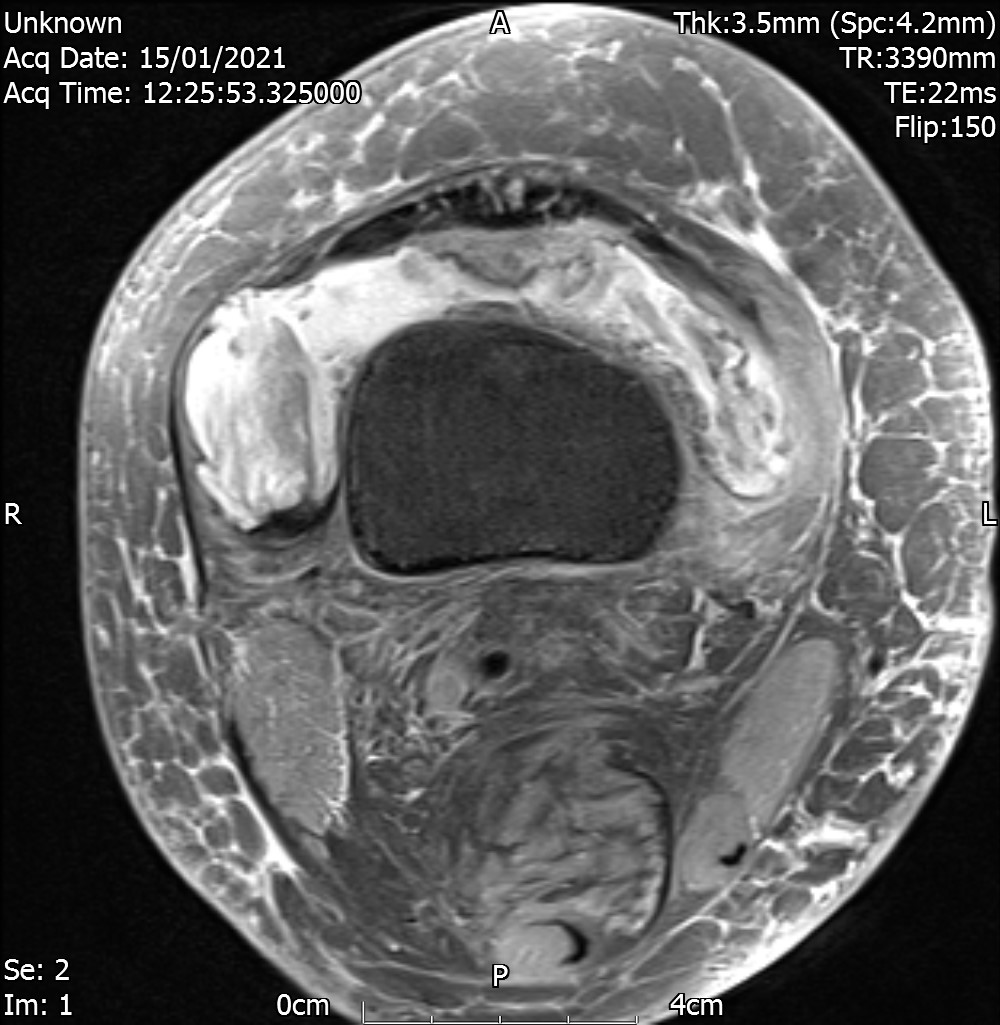
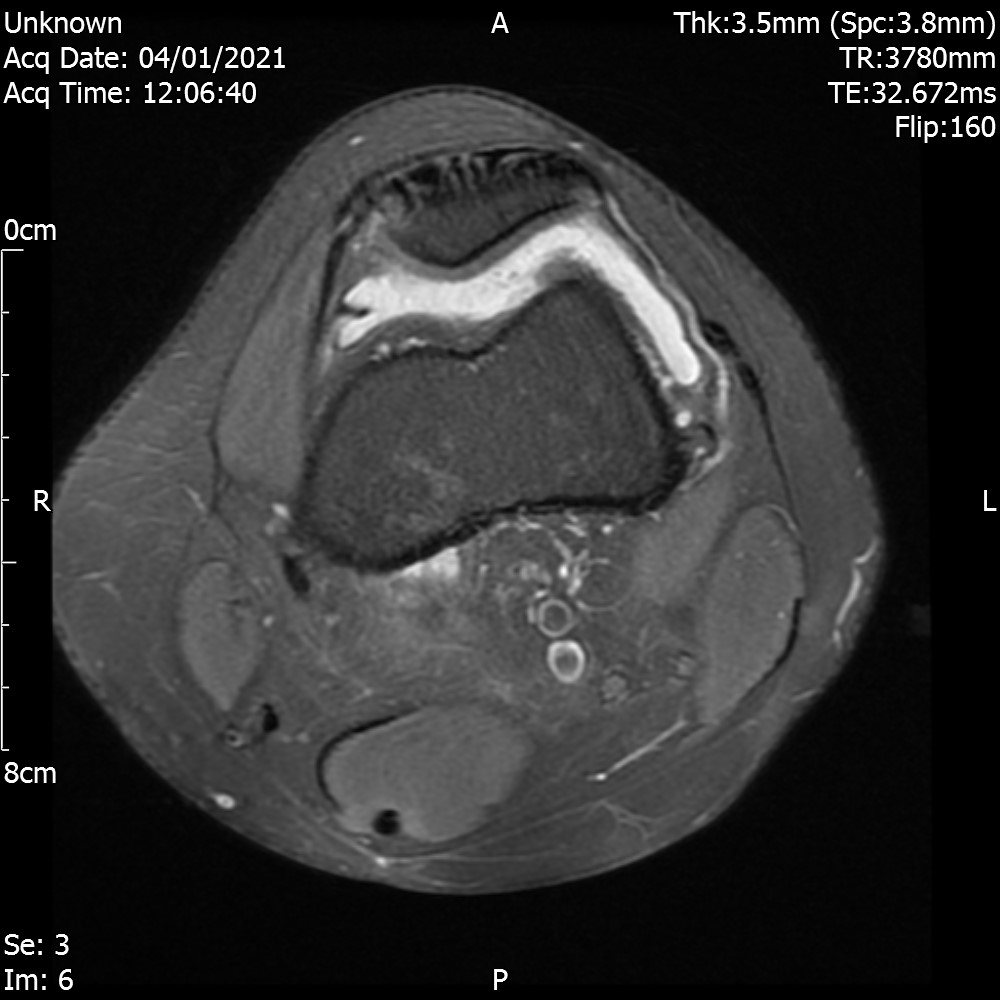
The MRI reports severe PFJ OA, massive joint effusion with suggestion of fatty synovial proliferation raising the possibility of lipoma arborescens. No meniscal or ligamentous tear is reported.
MRI – Saggital Views
MRI – Coronal Views
MRI – Axial Views
The patient is referred to an Orthopedic surgeon. The surgeon requests further MRI scan as the full extent of the lipoma is not visible. Lipoma arborescens is confirmed as a diagnosis and the surgeon refers the case to a sarcoma unit who then excise the lipoma via a synovectomy. Pathology report reveals inflammation and the patient is referred to Rheumatology for further review.
Patient sees another physiotherapist (same senior clinician) post surgery who joins the dots and pens downs the case after a retrospective analysis and concludes the following :-
- When junior clinicians raise a concern, they should be given thorough consideration. Clinical findings can be overlooked in a rushed assessment (between patients).
- Any lump / suspected lump around the knee should be investigated sooner rather than later. Threshold for investigation should be low when any lump is suspected.
- High BMI makes physical examination difficult. Presence of knee swelling can hide growths underneath them. The MRI scan in this case reports large effusion.
- Diffuse nature and uniform presence of lipoma around the knee (as is apparent from the MRI images above) makes detection difficult on physical examination alone.
References:
Lipoma arborescens is a chronic, slow-growing, intra-articular lesion of benign nature, which is characterized by villous proliferation of the synovium, with replacement of the subsynovial connective tissue by mature fat cells. It usually involves the suprapatellar pouch of the knee joint. It is not a neoplasm but is rather considered a nonspecific reactive response to chronic synovial irritation, due to either mechanical or inflammatory insults
Lipoma arborescens is a chronic, slowly progressive intra-articular lesion characterised by villous lipomatous proliferation of the synovium, usually involving the suprapatellar pouch of the knee joint. It is an uncommon cause of intra-articular masses that presents as slowly progressive painless swelling of the joint, which persists for many years and is accompanied by intermittent effusions.
Lipoma arborescens – Singapore Medical Journal 2014
Lipoma arborescens is a very rare pseudo-tumoral lesion of unknown etiology, characterized by lipomatous infiltration of subsynovial stroma, bilateral involvement is exceptional, only eight cases are reported in the literature.
Lipoma arborescens is a rare condition of unknown aetiology with benign diffuse villous proliferation of the synovium characterised by replacement of the subsynovial tissue by mature adipocytes. The knee is the most commonly involved joint.
Lipoma arborescens: an unusual case of knee swelling – BMJ 2014
Arborescent lipoma is a rare benign intra-articular lesion characterized by diffuse replacement of synovial tissue by mature adipocytes, causing a villous lipomatous proliferation of the sinovial membrane.
Lipoma arborescens of the knee: a case report – RBO 2014
Lipoma arborescens is a rare intra-articular lesion,characterised by diffuse replacement of thesubsynovial tissue by mature fat cells, producing prominent villous transformation of the synovium.
Lipoma arborescens of the knee – JBJS (Br) 1998
Intra-articular lipomas are rare and very few cases have been reported in the knee. To the best of our knowledge, here we report the largest lipoma to have ever been observed in the knee. It is crucial to avoid the misdiagnose of lipoma arborescens, which is associated with degenerative joint disease. Lipoma is a homogeneous, ovoid, adipose tissue tumor that is contained within a fibrous capsule and not associated with previous disease.
Large intra-articular true lipoma of the knee- BMC Musculoskeletal Disorders 2019