White Blood Cells or WBCs are formed in
- Bone Marrow – Granulocytes and Monocytes are formed in bone marrow
- Lymph tissue – Lymphocytes and Plasma Cells are formed in lymph tissue i.e lymph glands, spleen, thymus, tonsils, and various lymphoid tissues in the body such as in the bone marrow, gut wall etc.
The WBCs formed in the bone marrow are stored within the bone marrow. They are specifically transported to site of infection / inflammation when needed and are deployed quickly.
Lymphocytes are mostly stored in the lymphoid tissues. They are in constant circulation. They are released along the lymph from lymph nodes and lymphoid tissue. After a few hours they pass out of blood and back in to tissues via diapedesis. Then they re-enter the lymph and then back in to the circulation. Therefore they circulate continuously throughout the body.
Types of Leukocytes
- Polymorphonuclear Neutrophils – 65%
- Polymorphonuclear Eosinophils – 2.3%
- Polymorphonuclear Basophils – 0.4%
- Monocytes – 5.3%
- Lymphocytes – 30%
- Plasma Cells (occasionally)
Platelets (thrombocytes) are fragments of another type of cells similar to WBC called megakaryocyte. Megakaryocytes are also formed in the bone marrow. A microlitre of blood contains 300,000 of these. They are replaced every 10 days, so 30,000 are formed every day per microlitre of blood.
Neutrophils, eosinophils and basophils have granular appearance and are therefore called granulocytes. These have multiple nuclei.
- Granulocytes and monocytes protect the body by ingesting the invading cell i.e. phagocytosis.
- Lymphocytes and plasma cells function work in connection with the immune system.
1 microlitre of blood contains 7000 WBC (compared to 5 million RBC).
Genesis of WBC
- Myeloblast [▶] Promyelocyte [▶] Megakaryocyte [▶] Platelets
- Myeloblast [▶] Promyelocyte [▶] Granulocytes (Neutrophils, Eosinophils, Basophils)
- Myeloblast [▶] Monocytes
- Lymphoblast [▶] Lymphocytes
WBCs in Action
- It is mainly the Neutrophils and Macrophages that attack invading organisms such as bacteria, viruses etc..
- Macrophages start their life as monocytes which are immature cells while they are in blood and have little ability to fight infections. Once they migrate to tissues, they swell up and turn in to macrophages and become extremely capable of defending against invading organisms.
- Neutrophils and monocytes squeeze through the pores of blood capillaries in to the affected tissue (process called diapedesis). Within the tissues they move via ameboid movement to reach the target cell. Chemotaxis drives these cells to the affected tissue. Inflammed tissues release various factors which guide the WBCs to the affected tissue (process is called chemotaxis). Chemotaxis is effective up to 100 micrometres. No tissue in the body is more than 50 micrometre away from a capillary, so it is quite effective in driving the WBCs to the site of inflammation.
Phagocytosis & Opsonization
Cellular ingestion of the invading agent is called phagocytosis. The neutrophils and macrophages enclose the invading agent from all sides. The enclosed particle then detaches from the cell wall and forms a free floating phagocytic vesicle called phagosome inside the cytoplasm. Most particles are then digested by the intracellular enzymes. Lysosomes within the macrophages contain proteolytic enzymes which help in digesting bacteria and foreign protein matter. The lysosomes in macrophages also contain lipases which can digest some bacteria such as tuberculosis bacillus. The lysosomes of neutrophils do not contain lipases. The neutrophils and macrophages also contain bactericidal agents which kill bacteria. This is helpful where some bacteria have protective coats around them whereby they can’t be digested by enzymes. The enzymes in the membrane of the phagosome form oxidising agents. In some there is a special organelle called peroxisome which forms these oxidising agents. The oxidising agents are superoxide, hydrogen peroxide (H2O2), and hydroxyl ions which are lethal to most bacteria. One of the enzymes also catalyses reaction between H2O2 and chlorine to form hypchlorite which is strongly bactericidal. Some bacteria like TB have coats which are resistant to lysosomal digestion and they can also resist the killing effects of neutrophils and macrophages.
- A neutrophil can phagocytize 3-20 bacteria but a macrophage can phagocytize up to 100 bacteria.
- Macrophages can even phagocytize larger particles such as whole RBCs, whereas neutrophils cannot phagocytize anything larger than a bacteria.
- Whereas a neutrophil gets inactivated after engulfing bacteria and itself dies, a macrophage can survive and function for many months after engulfing bacteria.
Antibodies adhere to foreign agents and make them susceptible for phagocytosis. To do this antibodies also attach to receptor on the phagocyte membrane via C3 molecule. This process is called opsonization.
Reticuloendothelial System
The combination of monocytes, free roaming macrophages in blood and macrophages fixed in tissues and a few specialised endothelial cells in bone marrow, spleen, lymph nodes is called the reticuloendothelial system.
Macrophages in Lymph Nodes – A bacteria that enters the tissue cannot be absorbed via the capillary membranes in to the blood. If they are not destroyed locally, they flow via lymph in to a lymph node. A large number of macrophages line the lymph sinuses and these phagocytose any particle entering via lymph to stop its spread to the body.
Alveolar Macrophages – A large number macrophages are present in alveoli. They phagocytose particles trapped in alveoli. If the particle cant be digested the macrophages form a giant cell capsule around it.
Liver Macrophages | Kupfer cells – Bacteria can also enter the body via the GI tract via the GI mucosa into the portal blood. The blood then passes through liver sinusoids before getting in to the general circulation. The liver sinusoids are lined with macrophage Kupfer cells which are so effective that almost none of the bacteria passes from portal blood in to the general circulation.
Macrophages in Spleen & Bone Marrow – If any pathogen enters the general circulation then macrophages in spleen and bone marrow phagocytize them when they come in contact with them. Spleen is similar to a lymph node, the only difference being that instead of lymph blood passes through spleen. As blood flows through the capillaries, it passes in to spleen tissue (pulp) as the capillaries are highly porous before returning in to venous sinuses. The splenic tissue and venous sinuses are lined with macrophages which clear debris from the blood including abnormal and old RBCs.
Leukopenia
Leukopenia is a condition in which the bone marrow produces very few WBCs. This makes a person susceptible to infections.
Human body has commensals especially in the mouth and GI tract. Any reduction in WBCs allows for invasion of adjacent tissues by the commensals. As a result within 2 days of bone marrow suppression of WBC production, ulcers may appear in mouth and colon or a respiratory infection might appear. Death can occur within a week if left untreated.
X-ray and gamma ray irradiation or exposure to certain drugs can cause aplasia of bone marrow resulting in subsequent infection.
Leukemia
Leukemia refers to excessive and uncontrolled production of WBCs. Myelogenous (pertaining to myeloblasts lineage) or lymphogenous (pertaining to lymphoblasts) cell mutation causes excessive production of abnormal WBCs. As a result they do not provide any protection against infections.
Types
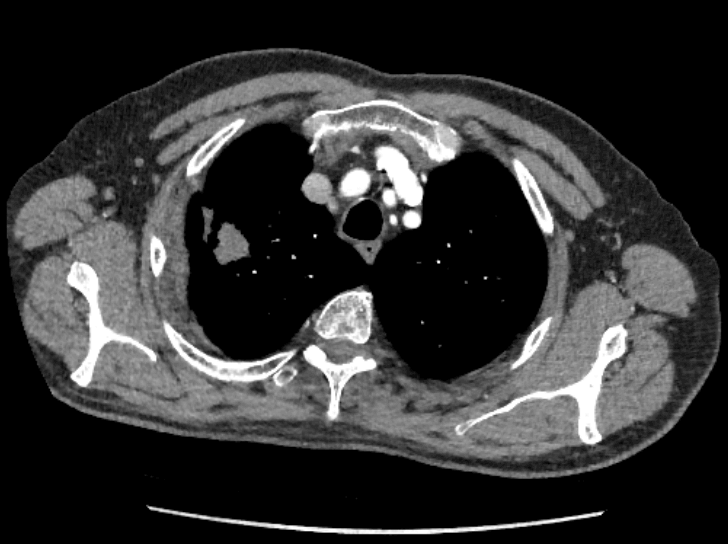
- Lymphocytic Leukemias – caused by cancerous production of lymphoid cells usually in lymph nodes or other lymphocytic tissues.
- Myelogenous Leukemias – caused by cancerous production of myelogenous cells in the bone marrow, but later on also in lymph nodes, spleen and liver.
Effects
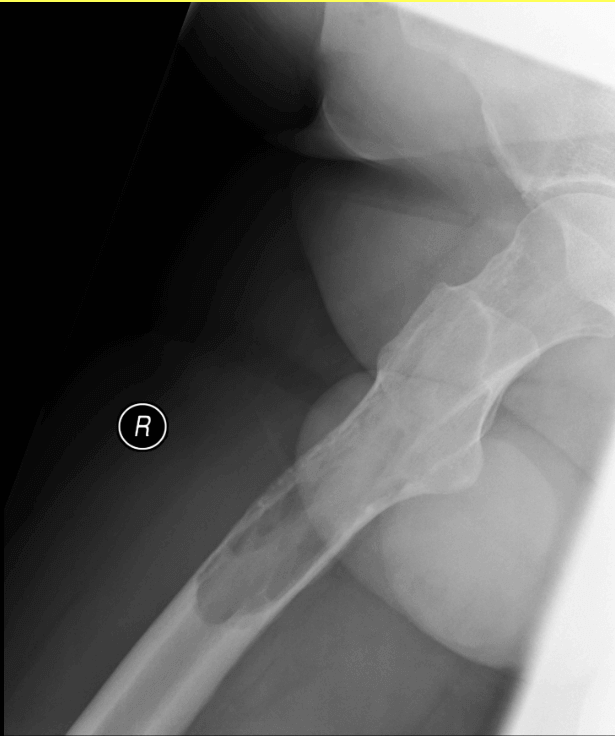
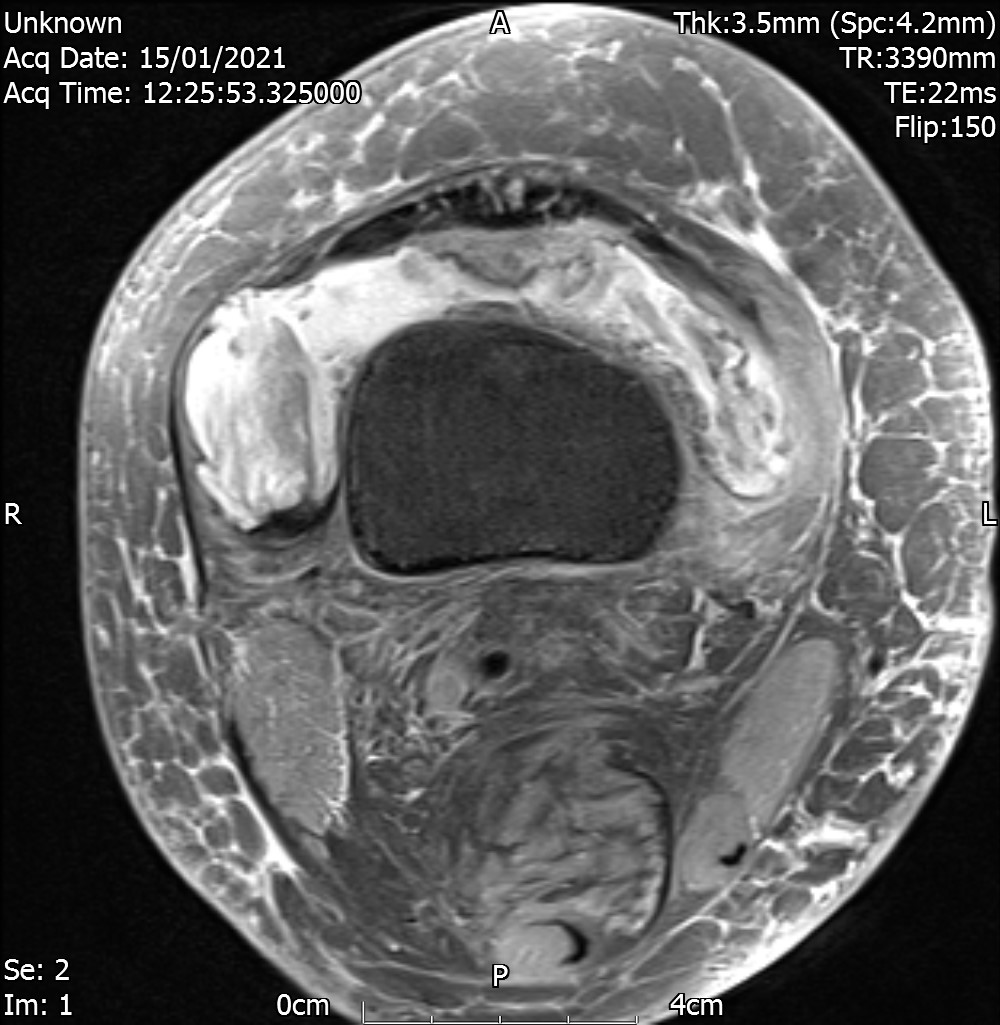
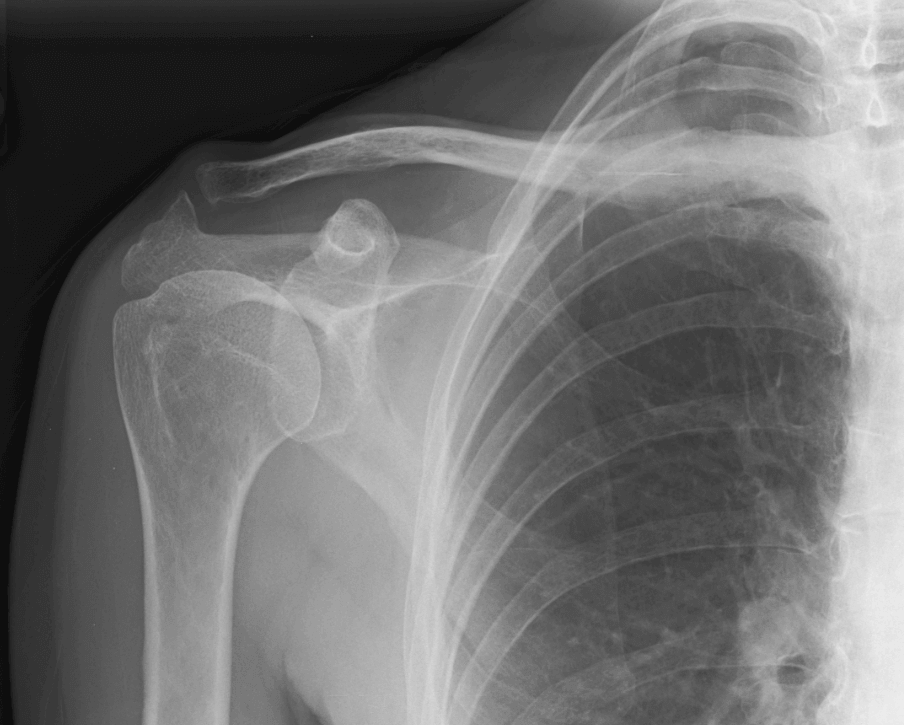
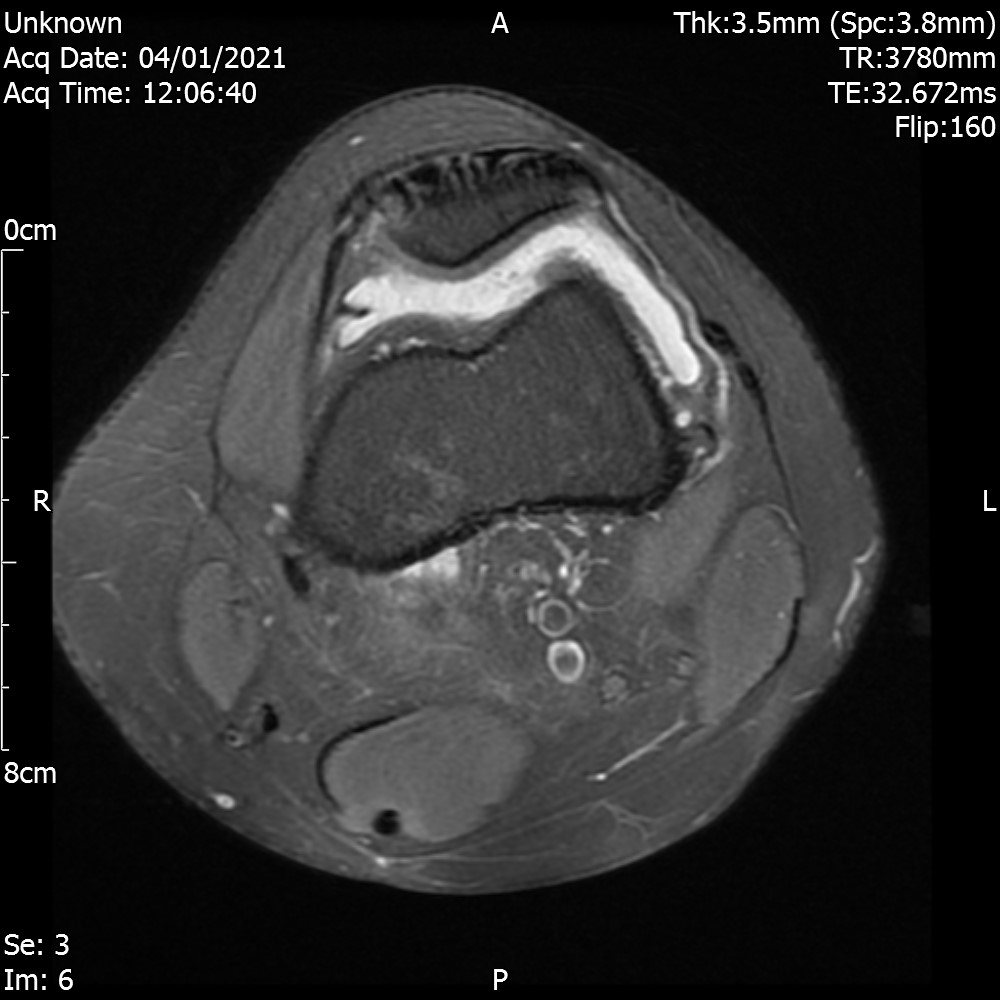
- Invasion of surrounding bone – excessive production of leukemic cells in bone marrow invade surrounding bone can cause pain and tendency for pathological fractures.
- Infections – due to leukopenia or reduction in normal WBCs which reduces immunity.
- Severe Anaemia – RBC production is reduced. This causes weakness and tiredness.
- Bleeding tendency due to thrombocytopenia as platelet production is reduced.
- Growing cancer cells consume a lot of food reserves especially amino acids and vitamins causing a depletion in energy and rapid deterioration of normal protein tissues. If this carries on for long, it can cause death.
The effects 2-4 happen because of reduction of normal bone marrow.